Nutrition
Diet and type 2 diabetes
Patient Information Leaflet
Introduction
This booklet gives some general information about what to eat and drink if you have type 2 diabetes. If you need more detailed advice, please ask your GP to refer you to a registered dietitian.
What is type 2 diabetes?
Type 2 diabetes occurs when the level of glucose (sugar) in the blood is too high.
In people without type 2 diabetes, a hormone called insulin helps to control blood glucose levels. Insulin acts like a key and allows glucose to move from the blood into the cells that make up your body. Your cells use glucose as fuel.
In people with type 2 diabetes, the main problem is that the insulin produced cannot work properly, which is known as insulin resistance. As time living with type 2 diabetes increases, the amount of insulin produced by the pancreas may also reduce. If diabetes has not yet been diagnosed or it is poorly controlled, high blood glucose levels may cause the following symptoms:
- Tiredness
- Excessive thirst.
- Weight loss.
- Passing water more often.
How is diabetes managed?
It is managed in one of four ways, depending on the person and the type of diabetes:
- Diet alone.
- Diet and tablets (for example, metformin and gliclazide).
- Diet and insulin.
- Diet, tablets and insulin.
Can type 2 diabetes be put into remission?
Recent evidence has shown that for many overweight or obese adults with type 2 diabetes, losing 15kg (2 stone 5lbs) as soon as possible after diagnosis is successful for achieving remission. Remission means that your blood glucose levels are below the diabetic range, usually without you needing to take any diabetes medication. If you feel this amount of weight loss is not realistic, but you would like to improve your blood glucose levels and reduce the risk of cardiovascular disease (CVD), it is recommended to lose at least five per cent of body weight if you are overweight or obese (i.e. body mass index, also known as BMI, more than or equal to 25 kg/m2).
Any dietary approach that results in weight loss could be suitable, particularly low-carb (less than 150g carbs daily), high-protein and Mediterranean. The most important factor is choosing the dietary approach that you can stick to long-term.
How can I keep my blood glucose levels in target?
The main food group that affects blood glucose levels is carbohydrates. Reducing carbohydrate consumption is one way to improve blood glucose control and lose weight.

Simple sugars
- Minimise these foods first (above in bold) to help control blood glucose.
- Replace sugar/honey in drinks and on food with artificial sweeteners. Speak to you dietitian if you have issues with diarrhoea or history of irritable bowel syndrome (IBS).
- Choose diet drinks or sugar-free versions.
Natural sugars
- Limit fruit to two to three small portions per day spread out. One portion is 80g, e.g. a fun-size banana, a medium apple, one quarter of a mango, a handful of grapes/berries.
- Milk and yogurt are a good source of calcium when eaten in moderation and should contribute to your recommended two to three portions of calcium per day (see advice on Calcium on page 4 of this leaflet). It is advised you opt for “no added sugar” or plain natural/Greek yogurt.
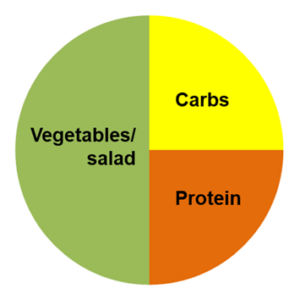 Starchy carbohydrates (yellow on the meal plate)
Starchy carbohydrates (yellow on the meal plate)
- Portion size is very important.
- Only have one portion at each meal and avoid double portions, e.g. pasta and garlic bread, burger bun and chips.
- For weight loss, aim to fill one quarter of your plate with starchy carbohydrates.
Suggested portion sizes:
- Two medium slices of bread.
- Four tablespoons of cooked rice/pasta/couscous.
- Four egg-sized new potatoes.
- One medium wrap/chapatti/pitta.
- Half of a fist-sized portion of fufu/plantain.
- Two slices of boiled yam.
- Choose high-fibre low glycaemic index (GI) carbohydrates, e.g. seeded or wholegrain bread, brown/long-grain/basmati rice, ideally wholegrain pasta or white pasta cooked firm, and porridge (made from jumbo oats).
- To the one quarter plate of carbohydrates, add a one quarter plate of protein (chicken, meat, fish, eggs, vegetarian alternatives, cheese, and beans) and a half plate of vegetables/salad.
Fibre
- It is recommended that we consume 30g of fibre per day.
- Fibre is found in wholegrain, starchy carbohydrates, fruit, vegetables, and legumes (beans, peas, lentils).
- Fibre helps to keep our bowels regular and healthy.
- If you are increasing your fibre intake, it is important to do so slowly to avoid unpleasant gastric side-effects and to also increase fluid consumption.
- It is advised to choose a wide variety of different vegetables of different colours to get different nutrients and support a healthy digestive system.
THE RAINBOW OF VEGETABLES

What are the other aspects of a healthy diet with diabetes?
Healthy fats
- Healthy fats are essential for life. These include oily fish, extra virgin olive oil, avocado, nuts and seeds.
- It is recommended that adults with diabetes consume two portions of oily fish per week, e.g. salmon, mackerel, sardines and pilchards.
- Nuts and seeds high in healthy fats include walnuts, almonds, macadamia nuts, hazelnuts, chia seeds, flaxseeds, sesame seeds
Calcium
- Calcium is important for healthy bones and teeth.
- Aim for two to three portions of calcium per day.
- One portion is:
- 200ml milk
- 150g Greek/plain/no added sugar yogurt
- 30g (matchbox-size) cheese
- One portion is:
What about physical activity?
-
- Any movement of your body will help lower blood glucose levels.
- It is recommended to do at least 150 minutes of moderate intensity activities (increased breathing, able to talk) per week e.g. swimming, brisk walking or cycling, or at least 75 minutes of vigorous intensity activities (breathing fast, difficulty talking) e.g. running, stair climbing or circuit training. You can also do a combination of both.
- Every minute counts.
- Minimise sedentary (sitting) time.
- On at least two days of the week, do activities to build strength, e.g. carrying heavy bags, yoga, using resistance bands or lifting weights.
- For older adults, to reduce the chance of frailty and falls, do activities to improve balance on two days per week, e.g. bowls, Tai Chi or dance.

Alcohol in moderation
- Alcohol recommendations for people with type 2 diabetes are the same as for the rest of the population, i.e. a maximum of 14 units per week for men and women.
- It is recommended to have two alcohol free days per week.
- A pint of 4% ale, lager, stout or normal strength beer contains two units, a 250ml large glass of red or white wine is three units and a 25ml shot of brandy, rum, vodka, gin or whisky is one unit.
- If you are trying to lose weight, reducing alcohol can also help as it contains “empty calories” (energy without nutrition).
- People with diabetes who take tablets and/or insulin should be aware that alcohol can cause blood glucose levels to decrease (hypoglycaemia). If you drink alcohol, the following advice will help you to make better choices and stay safe:
- Add diet pop or soda water to spirits.
- Alternate between diet soft drinks and alcoholic drinks during special occasions when you are drinking alcohol.
- Stick to smaller servings, for example, a 125ml glass of wine, half a pint, a single shot, a white wine spritzer with soda water.
- If you take tablets and/or insulin for your diabetes, reduce the risk of low blood glucose levels by eating before you drink alcohol, or drinking it at the same time as a meal. Then, eat a snack containing carbohydrates before going to bed.
- Let people around you know that you have diabetes and at risk of hypoglycaemia, so they can act accordingly if you show symptoms of dizziness, irritability, sweating. These can symptoms can mistaken for drinking excessive amounts of alcohol.
Meal ideas
Breakfast
- Porridge with milk and sweetener.
- One or two slices of granary toast with light olive spread, plus half a tin of reduced sugar baked beans or chopped tomatoes, two eggs (scrambled), peanut butter or 30g of cheese.
- 150g of Greek/natural/no added sugar yogurt, plus 80g of berries and a tablespoon of seeds or nuts.
- One or two slices of seeded toast, 1 egg with 20g of mozzarella cheese, 1 spoon of chia seeds.
Quick meals
- A sandwich made with two slices of seeded or granary bread, plus cucumber and tuna (tinned in spring water), cheese, ham or chicken and salad.
- Steamed mackerel from a tin, with a side salad including some pasta or potato.
- One wholemeal pitta bread stuffed with houmous, red pepper and salad leaves, or chicken and salad.
Cooked meals
- A piece of baked salmon with new potatoes and three tablespoons of mixed vegetables.
- Wholewheat spaghetti with homemade bolognese sauce, made with extra lean beef mince or Quorn mince, tinned chopped tomatoes and onion.
- Grilled chicken, red and yellow peppers and tomatoes flavoured with spices on a thin bed of basmati rice.
Desserts
- Sugar-free jelly with a handful of chopped fruit, or Greek/natural/no added sugar yoghurt.
- A small handful of tinned fruit (juice drained) with Greek/natural/no added sugar yoghurt.
- Two wholegrain crackers with cheese or peanut butter.
Snacks
Snacks are not essential, and if you are trying to lose weight, reducing snacks can be a good strategy.
If you are hungry, these are better suggestions:
- No added sugar yogurt (e.g. plain natural/Greek yogurt).
- Vegetable sticks, e.g. cucumber, celery, carrots and peppers (with or without hummus or peanut butter).
- A portion of fresh fruit (80g) or dried fruit (30g).
- Plain nuts (palm-sized portion or 25 to 30g).
- Two wholegrain crackers with meat/cheese/peanut butter.
- Two oatcakes with cheese/peanut butter.
- 200ml of milk.
- Small bar of dark chocolate (ideally more than 80%).
- Ice lollies made with diet drinks.
- Sugar-free jelly.
Can I find out more?
You can find out more on the Diabetes UK and NHS website:
If you have any questions, or if there is anything you do not understand, please contact the Russells Hall Hospital switchboard number on 01384 456111 and ask for the relevant department who issued this leaflet. If you have any feedback on this patient information leaflet please email dgft.patient.information@nhs.net
This leaflet can be made available in large print, audio version and in other languages, please call 0800 073 0510.
Originator: Nutrition and Dietetics Department. Date reviewed: April 2024. Next review due: Jan 2027. Version:4 DGH ref.: DGH/PIL/00975.
