Physiotherapy
Acute Low Back Pain
Patient Information Leaflet
Low Back Pain
This leaflet is designed to give you general advice to help you manage your lower back pain. More than 80 per cent of the general population suffer from simple back pain at some point in their lives, similar to getting a cold. Most acute back pain is the result of simple strains or sprains and the prognosis is excellent. Stress and mood can also affect your pain. Within the first two weeks of an acute episode of pain, most people will report a significant improvement in their symptoms with almost 85 per cent of people fully recovered by three months. Only a very small number of people develop long-standing, disabling problems.
If your back pain is severe and persistent after six weeks, please seek medical advice.
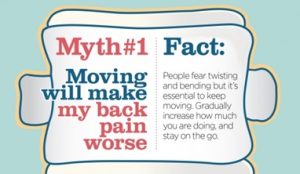
Most back pain will resolve, and staying active and continuing your usual activities will normally help with recovery. Research has shown that people who remain active get better more quickly, so bed rest is no longer recommended. This is because the spine needs movement to start to get better.
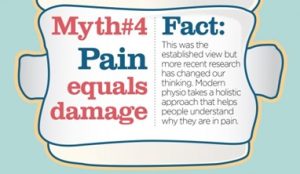
Remember: the back is a strong, robust structure which is designed to move to keep it healthy. The first few weeks may be painful, but this doesn’t always mean that harm is being caused. Following the advice below can help to manage this initial acute episode.
Low Back Pain Advice
Posture
Sit in a supportive comfortable chair and avoid low, soft chairs or sofas. You might like to use a rolled up towel in the small of your back to help support it. If you find a comfortable position such as lying on your front or sitting, use this position regularly throughout the day to reduce your symptoms. Remember that your spine likes movement, so try and change position every 20-30 minutes.
If you have to drive, make sure you take frequent breaks and adjust your car seat to the most comfortable position.
Sleeping
There is no right or wrong position for sleeping, and don’t worry about keeping your body in the same position all night. It’s normal for you to move around a bit when you sleep, and that’s a good thing as a little movement can help ease pressure off your back.
Medication
Pain relieving medication may be used to help keep you active and manage your symptoms in the short term. Please consult your pharmacist or GP if you are unsure what to take. Taking pain relief regularly can increase its effectiveness rather than ad hoc doses. Often over the counter medication is sufficient rather than stronger alternatives with other side effects.
Work
If you are having time off work, aim to return as soon as possible. Research has shown a quicker recovery if you return to work, than for those that stay at home.
If needed, discuss with your employer a staged return, or amendment of duties in the short term to assist you in getting back to work.
Stress / Mood
Stress, low mood and worry influence back pain. How we feel can influence the amount of pain we feel. Back pain can be triggered following changes in life, stress, mood or anxiety levels. In the same way that these factors are linked to other health conditions, such as cold sores, irritable bowel syndrome and tiredness, they also have a very large effect on back pain. As a result, managing our stress, mood and anxiety levels through doing things we enjoy and engaging in relaxation can be really beneficial in helping acute back pain.
Keeping Active
It is important to keep physically active as much as possible. Prolonged bed rest will make your symptoms worse.
Keeping active will:
- Prevent joint stiffness which can be a source of pain
- Reduce pain severity
- Keep your muscles strong
- Help you feel more positive
- Enable you to return to work more quickly
Types of Activity
Exercise is one of the best ways to help prevent and manage low back pain. The type of exercise does not matter, as long as you remain active. Below are some of the more common examples.
- Walking
- Swimming – the water environment takes the strain off joints and muscles while working out the entire body
- Yoga – strengthens muscles, increases flexibility and promotes relaxation
- Pilates – strengthens muscles and promotes good posture
- Dancing or aerobics
- Gym work / weights
- Mindfulness, meditation and relaxation are useful when combined with exercise
However, there are some gentle exercises that are recommended in the early stages to help get you moving. Do up to ten times each at regular intervals e.g. three times per day. They can improve your pain, but it is normal to experience a mild increase in symptoms.
• Lower Back Extension

Keep your hips down and relax your back. Push up with your arms to arch your back. Stop at the point where you feel a stretch in your lower back. Hold for a moment, and then slowly lower yourself back down.
- Knee Hugs

Lie on your back and gently bring one knee toward your chest and then the other. Use your arms to hug your knees in as close as you can manage comfortably. Hold for ten seconds if able.
- Leg Rolls

Keeping your knees together, drop them down to one side, rotating your torso. Return to the starting position and allow your knees to fall to the opposite side. Only drop as far as is comfortable. You may want to hold the stretch on each side.
- Arching and Hollowing

Start on your hands and knees.
Inhale, and arch your spine away from the floor, pulling your belly up like a cat.
When the time comes to exhale, round your spine in the opposite direction, lowering your belly towards the floor, and lifting your head. Rest for a few seconds, and then repeat.
It is a good sign if the above exercises reduce your pain or the pain moves to the centre of your back.
Stop the above exercises if your pain is getting progressively worse, particularly if pain transfers to the buttock or leg.
Seek Immediate Help
Seek immediate medical advice from your GP or emergency department if you develop any of the following symptoms:
- Loss of feeling/pins and needles between your inner thighs or genitals
- Numbness in or around your back passage or buttocks
- Altered feeling when using toilet paper to wipe yourself
- Increasing difficulty when you try to urinate
- Increasing difficulty when you try to stop or control your flow of urine
- Loss of sensation when you pass urine
- Leaking of urine or recent use of pads
- Not knowing when your bladder is either empty or full
- Inability to stop a bowel motion or leaking
- Loss of sensation when you pass a bowel motion
- Change in ability to achieve an erection or ejaculate
- Loss of sensation in genitals during sexual intercourse
Any combination or number of these warning signs could be symptoms of Cauda Equina Syndrome (CES). This is a rare condition. In patients with CES, something presses on a bundle of spinal nerve roots called Cauda Equina. These nerves are at the lower end of the spinal cord, and they send and receive messages to and from your legs, feet, and pelvic organs.
Remember: most back pain does get better. It just takes a little time.
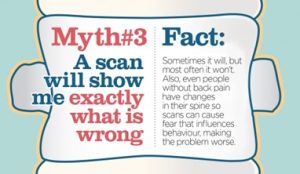
Back Pain Myth Busters

Further Information and References
NICE: Please see the below link to see what treatment and care you can expect from the NHS for your Low Back Pain.
https://www.nice.org.uk/guidance/NG59
www.patient.co.uk – back pain
If you have any questions, or if there is anything you do not understand about this leaflet, please contact:
Community Physiotherapy: 01384 321605
Russells Hall Hospital switchboard number: 01384 456111
If you have any feedback on this patient information leaflet, please email dgft.patient.information@nhs.net
Date reviewed: October 2025 Next review date: October 2028 Version: 2
