Ophthalmology
Aflibercept (Eylea) for age-related macular degeneration (ARMD)
Patient Information Leaflet
Introduction
Your eye doctor has already given you a patient information leaflet called ‘Your guide to age-related macular degeneration’ describing the various forms of age-related macular degeneration (ARMD) and their treatment.
This leaflet contains detailed information on a treatment with the medical name of ‘aflibercept,’ also known as Eylea. The leaflet includes information on the procedure, the risks and the benefits.
If you suffer from glaucoma / ocular hypertension and have been enlisted for intravitreal Aflibercept (Eylea) injections, please continue to take your prescribed glaucoma eye drops whilst having these injections.
What is Aflibercept (Eylea)?
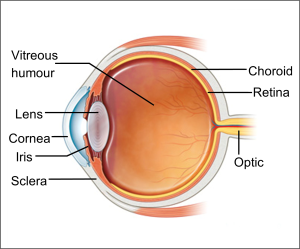
If your doctor is suggesting Eylea treatment, it means your eye contains extra amounts of a protein called vascular endothelial growth factor (VEGF). It is one of the causes of leaky, abnormal blood vessels. The excess fluid that comes from these blood vessels can build up and lead to reduction in your vision.
Eylea is designed to block VEGF. By blocking VEGF, Eylea may prevent damaged blood vessels from leaking fluid into the macula. It is given by a course of injections into the eye. Long term, the number of injections will depend on how the ARMD responds to the treatment.
Your doctor has found that you have the wet form of ARMD, and need to be started on eye injections to treat it.
These injections are currently the most effective treatment for wet ARMD. They work by penetrating into the nerve layer at the back of the eye (the retina). The macula is the most important part of the retina and is responsible for your central vision. Over time, the injections close up the leaking blood vessels affecting the macula, which should reduce the swelling in the macula and hopefully improve your vision.
Since 2008, we have been using Ranibizumab (Lucentis) for the treatment of wet ARMD. In 2013, Aflibercept (Eylea) was approved by The National Institute for Health and Care Excellence (NICE) for this condition.
Although Aflibercept (Eylea) is equally as effective as Ranibizumab (Lucentis), reports have shown that it has a beneficial effect when used in some patients who have stopped responding to repeated treatments of Ranibizumab (Lucentis). Eylea can be used either as a new treatment or as a replacement for when Ranibizumab (Lucentis) stops working as efficiently. It has a longer lasting effect on retinal conditions which means it can be used less frequently for the same beneficial effect.
In 2022 an even longer acting anti VEGF injection was launched (Faricimab). You can discuss with your eye doctor the various injection options.
In either case, you will be receiving three Aflibercept (Eylea) injections, once every month for the first three months (this is called a loading dose), followed by a fixed regimen of an injection every two months in year one. In the subsequent years, the injection is given as and when required, just like Ranibizumab (Lucentis). The number and frequency of the injections and the overall duration of treatment depends on the diagnosis and severity of the condition. Many patients have to have the injections for up to three years or longer. Your doctor will choose and discuss the treatment plan (regimen) best suited to your eye.
How long am I consenting for treatment?
You will be given an indefinite course of treatment, unless you withdraw consent or lose capacity.
What happens during the treatment?
You should not feel any pain during the eye injections, since your eye is numbed with anaesthetic drops prior to the injections. You may feel some pressure on your eye. You will not need to stay in hospital.
After the treatment
You can take a couple of paracetamol tablets (500mg) in the morning of the injection or afterwards (if not allergic) if necessary.
Please continue to take any other eye drops that you already use (e.g. for glaucoma or dry eye). After the injection, the eye will be covered by an eye shield to prevent corneal scratch / abrasion. Please keep the shield on the eye until the next morning.
Will my vision improve with the injection?
About 95 per cent of people with wet ARMD treated with Aflibercept (Eylea) in the clinical trials found that their vision either improved or stabilised after one year of treatment. About one third of patients found that their vision was much better than before treatment.
What are the benefits?
The benefits of the treatment are:
- The injections should reduce inflammation and swelling in the macula of your eye.
- It can also help improve vision and prevent further damage.
What are the risks of having the injections?
You need to know about the side effects. Most treatments have some risks. The risks of Eylea are as follows:
Common risks (one person out of 10 may get these):
- Blood shot eye (sub-conjunctival haemorrhage).
- Damage to the front of the eyeball (corneal scratch).
- Raised intra-ocular pressure.
- Injection site pain and foreign body sensation.
- Risk of retinal pigment epithelium (RPE) tear in large pigment epithelial detachment (PED).
- As with all anti-VEGF injections, thrombo-embolic events (stroke / mini stroke / TIA (transient ischaemia attack)) have been reported in studies. However, it is not clear if this is due to the injections or the age-related ill health of the patients undergoing the treatment.
Uncommon risks (one person out of 100 may get these):
- Allergic reactions (hypersensitivity).
- Inflammation (iritis).
Rare risks (one person out of 1000 may get these):
- Less than 0.5 per cent of patients may have an eye infection (Endophthalmitis), leading to complete loss of vision (blindness).
- Lens trauma leading to a cataract.
- Detachment of the retina and / or vitreous.
What are the alternatives?
Currently, other licensed anti-VEGF treatments for wet ARMD apart from Aflibercept (Eylea), are Ranibizumab (Ongavia) and Faricimab (Vabysmo) intravitreal injections.
Is there any reason why I cannot have the injections?
- The injections cannot be given to people who have had a stroke, mini-stroke (TIA) or heart failure in the past three months.
- They will not be used in the presence of infection / inflammation in or around the surrounding tissues of the eye.
- They will not be used 28 days prior to or after other intra-ocular surgery.
- The injections are unsuitable in pregnancy and breast feeding women.
- Additional support may be needed for patients who may find local anaesthetics difficult to tolerate due to dementia/cognitive impairment. In this case, alternative solutions will be discussed with the patient and those who support them.
‘One Stop Service’
The Trust is introducing a ‘One Stop Service’ for some intravitreal injections. A ‘One Stop Service’ is where an injection may be offered on the same day you attend the eye clinic. This may result in you having an extended waiting time in clinic, but it will mean you do not have to return on a separate occasion for your eye injection. A doctor or nurse will discuss this with you in the clinic.
Advice after eye injections
What should I expect after the injection?
Your eye may feel painful for 24 to 48 hours. If necessary, you can take painkillers such as paracetamol or ibuprofen if you can take them (always read the label; do not exceed the recommended dose). If the eye becomes significantly red and painful with reduced vision, contact the Urgent Referral team immediately on 01384 456111 ext. 3633.
It is best to avoid products containing aspirin. However, if you take regular soluble aspirin (75mg), you can continue to take it as advised by your GP.
If you have bruising on or around the eye, this should fade gradually over the next couple of weeks.
At times, a tiny air bubble can be introduced into the eye during the injection. This appears as a round, dark floater in the centre of your vision the day after the injection. Do not be alarmed, as this will get smaller and should disappear within 48 hours.
Rarely, the surface of the eye can get scratched during the injection process. This can cause sharp, sudden pain three to six hours after the injection. If this happens, it is easy to treat, so please get in touch with the Urgent Referral team at Russells Hall Hospital Eye Clinic on 01384 456111 ext. 3633 (9am to 4.30pm, Monday to Friday).
What do I need to do?
If you have an eye pad to prevent the cornea from being scratched or damaged, you can gently remove this the next morning. The eye pad may be slightly bloodstained, but this is nothing to worry about.
You can clean your eye the morning after your injection with cool, boiled water and a small piece of cotton wool or lint. Close your eye first, and then gently wipe from the inner corner of the eye to the outer corner of the eye, using a fresh piece of cotton wool or lint each time and for each eye.
If you were prescribed antibiotic drops to use at home, continue to use them for five days. If you have been prescribed glaucoma eye drops, you should use them on the morning of the injection, but not after the injection for the rest of that day. The next day you should start your glaucoma eye drops again using a new bottle.
What if I have any problems or questions after reading this leaflet?
Please contact the Urgent Referral Clinic team at Russells Hall Hospital Eye Clinic on 01384 456111 ext. 3633 (9am to 4.30pm, Monday to Friday).
Eye emergency, out of hours
In case of an eye emergency after the closing hours of the Eye Clinic at
Russells Hall Hospital (including weekends and bank holidays), please contact:
Birmingham and Midland Eye Centre on 0121 507 4440
The doctor on call is usually based at the Eye Centre, City Hospital, Dudley Road, Birmingham. They may need to call you back, and if necessary, they will arrange for you to visit them.
Where can I find out more?
You can find out more from the following web-link:
NHS Choices
http://www.nhs.uk/Conditions/Macular-degeneration/Pages/introduction.aspx
Note: the information in this booklet is provided for information only. The information found is not a substitute for professional medical advice or care by a qualified doctor or other health care professional. Always check with your doctor if you have any concerns about your condition or treatment. This is only indicative and general information for the procedure. Individual experiences may vary and all the points may not apply to all patients at all times. Please discuss your individual circumstances with your eye doctor.
Author: Mr S Shafquat FRCS FRCOphth, Consultant Ophthalmologist, Retina Lead
If you have any questions, or if there is anything you do not understand, please contact the Russells Hall Hospital switchboard number on 01384 456111 and ask for the relevant department who issued this leaflet.
If you have any feedback on this patient information leaflet please email dgft.patient.information@nhs.net
This leaflet can be made available in large print, audio version and in other languages, please call 0800 073 0510.
Eylea/ARMD/SS/ST/11 2024/v6 – review 08 2027 DGH/PIL/02085