Ophthalmology
Intravitreal triamcinolone acetonide (Intracinol) injection
Patient Information Leaflet
Introduction
Your doctor has found that you have leakage of blood vessels, causing swelling at the back of your eye (the macula). This occurs as a result of different conditions, including diabetes, blockage of veins at the back of the eye, after cataract surgery, eye inflammation and abnormal vessels (macular telangiectasia, also known as “MacTel”). If left untreated, this may result in permanent reduction in your vision in that eye.
This leaflet contains detailed information on a treatment with the medical name triamcinolone acetonide (IVTA), also known as Intracinol. This leaflet includes information on the procedure, the risks and the benefits.
To reduce this swelling, you need to be started on these eye injections. They work by penetrating into the nerve layer at the back of the eye (the retina). The macula is the most important part of the retina, which is responsible for central vision. Over time, the injections close up the leaking blood vessels affecting the macula, which should reduce the swelling in the macula, and hopefully improve your vision.
What is intravitreal triamcinolone acetonide – IVTA (Intracinol)?
Triamcinolone acetonide (trade name Intracinol) is a steroid injected into the jelly (vitreous) part of the eye.
It has been shown to reduce the swelling and leakage of blood vessels at the macula, and it may improve how well you see.
Intracinol is approved by the Medicines and Healthcare products Regulatory Agency (MHRA) for use in the eye.
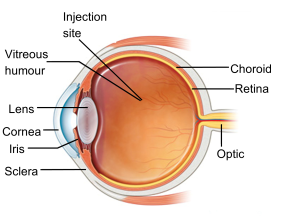
Figure 1 shows the side image of an eye (image courtesy of NHS Choices)
Depending on how the eye responds, these injections may be given on multiple occasions over the coming months in the affected ey
Wil my vision improve with the injection?
In most cases, the injection is capable of reducing retinal swelling and inflammation, leading to improved vision. The beneficial effects of the injection can be short-lived, as the drug lasts six to eight weeks.
How long am I consenting for treatment?
You will be given an indefinite course of treatment, unless you withdraw consent or lose capacity.
What are the benefits?
As mentioned in the above paragraph, the injection is capable of reducing retinal swelling and inflammation.
What are the risks of having the injection?
You need to know about the possible side effects:
- Less than 0.5 per cent of patients may have an eye infection (Endophthalmitis), leading to complete loss of vision (blindness).
- You may have a retinal detachment or cataract as a result of the injection.
- Between 28 per cent and 77 per cent (28 to 77 out of 100) of patients may experience an increase in intraocular pressure as a result of the injection. This is more likely if you have high intraocular pressure before the injection or if a higher dose is injected.
- Any of these complications may lead to blindness. Additional medications or procedures (including surgery) may be needed to treat these complications.
Other less serious side effects include pain, subconjunctival haemorrhage (blood shot eye), floaters in your vision, damage to the retina or cornea (structures of the eye), inflammation of the eye and bleeding. Again, additional medications or procedures may be required to treat these side effects.
Other possible limitations
The goal of treatment is to prevent any further loss of vision. Although some patients have regained vision, the medication may not restore vision that has already been lost, and may not ultimately prevent further loss of vision caused by your disease.
What are the alternatives to the injection?
Your doctor will be happy to discuss alternative treatments, although these may not be as effective in controlling your condition, or may have more serious side effects than the Intracinol injection.
Other alternatives include longer-acting intravitreal steroid injections (lluvein, Ozurdex), laser treatment (which may have already been given) and other types of injection called anti-vascular endothelial growth factor (anti-VEGF) therapy.
What happens before the treatment?
Please take your usual medication and eye drops on the day of your injection appointment. Before your injection, you will be given a tablet and eye drops to lower your eye pressure. If you want, you can take paracetamol tablets on the morning of the injection, if you can take them (always read the label; do not exceed the recommended dose).
What happens during the treatment?
You should not feel any pain during the eye injections, since your eye is numbed with anaesthetic drops prior to the injections. You may feel some pressure on your eye. You will not need to stay in hospital.
What happens after the treatment?
Most patients will not have any eye drops after the injection, however a small number of patients may be given antibiotic drops for five days after the treatment. Your doctor will discuss this with you. You can take a couple of paracetamol tablets (500mg) in the morning of the injection or afterwards (if not allergic) if necessary.
Please continue to take any other eye drops that you already use (such as, for glaucoma).
After the injection, the eye will be covered by an eye shield to prevent corneal scratch / abrasion. Please keep the shield on the eye until the next morning.
Frequently, patients see a dark, cloudlike floater in their vision a week after the injection. This is produced by the drug triamcinolone (Intracinol) in the jelly of the eye.
Client consent
The nature of my eye condition has been explained to me and the proposed treatment has been described. The risks, benefits, alternatives, and limitations of the treatment have been discussed with me. All of my questions have been answered.
- I will take all prescribed medications exactly as prescribed and will immediately contact my doctor if the following signs of infection or other complications develop:
- Pain
- Blurry or decreased vision
- Sensitivity to light
- Redness of the eye
- Discharge from the eye
I have been instructed not to rub my eye or swim for five days after the injection. I will keep all post-injection appointments so my doctor can check for complications. I have been instructed not to drive to my hospital appointment and not to drive later on the same day.
Is there any reason why I cannot have the injection?
- The injection cannot be given to people who have glaucoma or significant increased eye pressure.
- It will not be used if you have an infection or inflammation in or around the surrounding tissues of the eye.
- Additional support may be needed for patients who may find local anaesthetic difficult to tolerate due to cognitive impairment. In this case, alternative solutions will be discussed with the patient and those who support them.
Advice after eye injections
What should I expect after the injection?
Your eye may feel painful for 24 to 48 hours. If necessary, you can take painkillers such as paracetamol or ibuprofen if you can take them (always read the label; do not exceed the recommended dose). If the eye becomes significantly red and painful with reduced vision, contact the Urgent Referral team immediately on 01384 456111 ext. 3633.
It is best to avoid products containing aspirin. However, if you take regular soluble aspirin (75mg), you can continue to take it as advised by your GP.
If you have bruising on or around the eye, this should fade gradually over the next couple of weeks.
At times, a tiny air bubble can be introduced into the eye during the injection. This appears as a round, dark floater in the centre of your vision the day after the injection. Do not be alarmed, as this will get smaller and should disappear within 48 hours.
Rarely, the surface of the eye can get scratched during the injection process. This can cause sharp, sudden pain three to six hours after the injection. If this happens, it is easy to treat, so please get in touch with the Urgent Referral team at Russells Hall Hospital Eye Clinic on 01384 456111 ext. 3633 (9am to 4.30pm, Monday to Friday).
What do I need to do?
If you have an eye pad to prevent the cornea from being scratched or damaged, you can gently remove this the next morning. The eye pad may be slightly bloodstained, but this is nothing to worry about.
You can clean your eye the morning after your injection with cool, boiled water and a small piece of cotton wool or lint. Close your eye first, and then gently wipe from the inner corner of the eye to the outer corner of the eye, using a fresh piece of cotton wool or lint each time and for each eye.
If you were prescribed antibiotic drops to use at home, continue to use them for five days. If you have been prescribed glaucoma eye drops, you should use them on the morning of the injection, but not after the injection for the rest of that day. The next day you should start your glaucoma eye drops again using a new bottle.
What if I have any problems or questions after reading this leaflet?
Please contact the Urgent Referral Clinic team at Russells Hall Hospital Eye Clinic on 01384 456111 ext. 3633 (9am to 4.30pm, Monday to Friday).
Eye emergency, out of hours
In case of an eye emergency after the closing hours of the Eye Clinic at
Russells Hall Hospital (including weekends and bank holidays), please contact:
Birmingham and Midland Eye Centre on 0121 507 4440
The doctor on call is usually based at the Eye Centre, City Hospital, Dudley Road, Birmingham. They may need to call you back, and if necessary, they will arrange for you to visit them.
Note: the information in this booklet is provided for information only. The information found is not a substitute for professional medical advice or care by a qualified doctor or other healthcare professional. Always check with your doctor if you have any concerns about your condition or treatment. This is only indicative and general information for the procedure. Individual experiences may vary and all the points may not apply to all patients at all times. Please discuss your individual circumstances with your eye doctor.
Author: Mr S Shafquat FCPS FRCS FRCOphth Consultant Ophthalmologist, Retina Lead
If you have any questions, or if there is anything you do not understand, please contact the Russells Hall Hospital switchboard number on 01384 456111 and ask for the relevant department who issued this leaflet.
If you have any feedback on this patient information leaflet please email dgft.patient.information@nhs.net
This leaflet can be made available in large print, audio version and in other languages, please call 0800 073 0510.
IVTA Intracinol/SS/AW/ST/11 2024/v3 – review 08.2027 DGH ref.: DGH/PIL/02160
