Ophthalmology
Ranibizumab (Ongavia) and Aflibercept (Eylea) treatment for pathological myopia (PM)
*Ranibziumab (Ongavia) is a highly similar copy of the original Ranibizumab molecule. The World Health Organisation (WHO) defines biosimilar as a medicine that is similar in terms of quality, effectiveness and safety to the original licensed product.
The information within this leaflet is from Ranibizumab (Lucentis) studies but applies equally to the biosimilar drug (Ongavia).
Patient Information Leaflet
Introduction
This leaflet describes the latest treatments (Ongavia or Eylea injections given into the eye) available to you.
The doctor has found that you have either a retinal haemorrhage or a swelling affecting the centre of the retina, from pathological myopia (short-sightedness). These injections are currently the most effective approved treatment for pathological myopia. They work by penetrating into the nerve layer at the back of the eye (the retina). The macula is the most important part of the retina and is responsible for your central vision. Over time, the injection/s close up the leaking blood vessels affecting the macula, which should reduce the swelling in the macula and hopefully improve your vision.
Depending on the response, these injections may be given on multiple occasions in the affected eye.
If you suffer from glaucoma / ocular hypertension and have been enlisted for intravitreal Ranibizumab (Ongavia) / Aflibercept (Eylea) injections, please continue to take your prescribed glaucoma eye drops whilst having these injections.
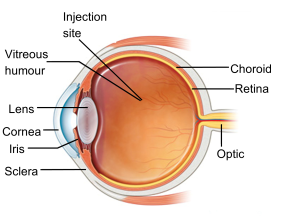
Figure 1 shows the side image of an eye (image courtesy of NHS Choices)
How long am I consenting for treatment?
You will be given an indefinite course of treatment, unless you withdraw consent or lose capacity.
Wil my vision improve?
These two injections are currently the most effective treatment for central retinal haemorrhage associated with pathological myopia. They are also recommended by NICE (National Institute for Health and Clinical Excellence).
What are the benefits?
Both types of anti-vascular endothelial growth factor (anti-VEGF) injections act by reducing inflammation, fluid (swelling) and slowing down leakage of fluid from abnormal retinal vessels.
What are the risks of having the injections?
You need to know about the side effects:
- Up to three and a half per cent of patients may have a stroke or mini-stroke during the three-year course, but it is not clear if this is due to the injections or the age-related frailty of the patients undergoing the treatment.
- Raised blood pressure (hypertension) is seen in up to eight per cent.
- Nose bleeds have been reported in one per cent.
- Conjunctival haemorrhage is seen in seven per cent.
- Less than 0.5 per cent of patients may have an eye infection (Endophthalmitis), leading to complete loss of vision (blindness).
- Raised intra-ocular pressure in the eye.
- Very rarely, the injection needle can touch the lens, producing an opacity (cataract), or touch the retina, producing a retinal tear / detachment.
What are the alternatives?
Your doctor will be happy to discuss alternative treatments. Currently, however, there are no other more effective treatments recommended.
What happens before the treatment?
Please take your usual medication and eye drops on the day of your injection appointment. If you want, you can take paracetamol tablets on the morning of the injection, if you can take them (always read the label; do not exceed the recommended dose).
What happens during the treatment?
You should not feel any pain during the eye injections as your eye is numbed with anaesthetic drops prior to the injections. You may feel some pressure on your eye. You will not need to stay in hospital.
What happens after the treatment?
Most patients will not have any eye drops after the injection. However, a small number of patients may be given antibiotic drops for five days after the treatment. Your doctor will discuss this with you. You can take a couple of paracetamol tablets (500mg) on the morning of the injection or afterwards (if not allergic) if necessary.
Please continue to take any other eye drops that you already use (such as for glaucoma). After the injection, your eye will be covered by an eye shield to protect it. Please keep the shield on the eye until the next morning.
Is there any reason why I cannot have the injections?
- The injections cannot be given to people who have had a stroke, mini-stroke or heart failure in the past four months.
- It will not be used in the presence of infection / inflammation in or around the surrounding tissues of the eye.
- Ranibizumab (Ongavia) or Aflibercept (Eylea) are unsuitable for pregnant or breastfeeding patients.
- Female patients of child bearing age must use contraception if they are to have either injection due to the potential harmful effects on the fetus (teratogenic effects).
- Additional support may be needed for patients who may find local anaesthetic difficult to tolerate due to cognitive impairment. In this case, alternative solutions will be discussed with the patient and those who support them.
Advice after eye injections
What should I expect after the injection?
Your eye may feel painful for 24 to 48 hours. If necessary, you can take painkillers such as paracetamol or ibuprofen if you can take them (always read the label; do not exceed the recommended dose). If the eye becomes significantly red and painful with reduced vision, contact the Urgent Referral team immediately on 01384 456111 ext. 3633.
It is best to avoid products containing aspirin. However, if you take regular soluble aspirin (75mg), you can continue to take it as advised by your GP.
If you have bruising on or around the eye, this should fade gradually over the next couple of weeks.
At times, a tiny air bubble can be introduced into the eye during the injection. This appears as a round, dark floater in the centre of your vision the day after the injection. Do not be alarmed, as this will get smaller and should disappear within 48 hours.
Rarely, the surface of the eye can get scratched during the injection process. This can cause sharp, sudden pain three to six hours after the injection. If this happens, it is easy to treat, so please get in touch with the Urgent Referral team at Russells Hall Hospital Eye Clinic on 01384 456111 ext. 3633 (9am to 4.30pm, Monday to Friday).
What do I need to do?
If you have an eye pad to prevent the cornea from being scratched or damaged, you can gently remove this the next morning. The eye pad may be slightly bloodstained, but this is nothing to worry about.
You can clean your eye the morning after your injection with cool boiled water and a small piece of cotton wool or lint. Close your eye first, and then gently wipe from the inner corner of the eye to the outer corner of the eye, using a fresh piece of cotton wool or lint each time and for each eye.
If you were prescribed antibiotic drops to use at home, continue to use them for five days. If you have been prescribed glaucoma eye drops, you should use them on the morning of the injection, but not after the injection for the rest of that day. The next day you should start your glaucoma eye drops again using a new bottle.
What if I have any problems or questions after reading this leaflet?
Please contact the Urgent Referral Clinic team at Russells Hall Hospital Eye Clinic on 01384 456111 ext. 3633 (9am to 4.30pm, Monday to Friday).
Eye emergency, out of hours
In case of an eye emergency after the closing hours of the Eye Clinic at Russells Hall Hospital (including weekends and bank holidays), please contact:
Birmingham and Midland Eye Centre on 0121 507 4440
The doctor on call is usually based at the Eye Centre, City Hospital, Dudley Road, Birmingham. They may need to call you back, and if necessary, they will arrange for you to visit them.
Note: The information in this booklet is provided for information only. The information found is not a substitute for professional medical advice or care by a qualified doctor or other health care professional. Always check with your doctor if you have any concerns about your condition or treatment. This is only indicative and general information for the procedure.
Individual experiences may vary and all the points may not apply to all patients at all times. Please discuss your individual circumstances with your eye doctor.
Author: Mr S Shafquat FRCS, FRCOphth Consultant Ophthalmologist, Retina Lead
If you have any questions, or if there is anything you do not understand, please contact the Russells Hall Hospital switchboard number on 01384 456111 and ask for the relevant department who issued this leaflet.
If you have any feedback on this patient information leaflet please email dgft.patient.information@nhs.net
This leaflet can be made available in large print, audio version and in other languages, please call 0800 073 0510.
LucentisPM/SS/AW/ST/11.2024/v4 – review 08.2027 – DGH ref.: DGH/PIL/02137