Renal (Haemodialyis & Peritoneal Unit)
The arteriovenous fistula for haemodialysis
Patient Information Leaflet
Introduction
The information contained in this booklet is for:
- Patients waiting to go on the haemodialysis programme.
- Patients with a temporary or permanent catheter already having haemodialysis.
- Patients on the continuous ambulatory peritoneal dialysis program (CAPD) transferring to haemodialysis.
- Patients waiting for another permanent vascular access device to be fitted.
It contains information on what an arteriovenous fistula is, how one is fitted, how to look after it once it is in place and what to do if you have any problems.
Please note that the information in this booklet is only a guide. If you need any more information or have any queries, please speak to the Renal Unit staff.
Your fistula is your lifeline. Please look after it.
What is haemodialysis?
People who have chronic kidney disease (CKD) have lost the normal functions of one or both of their kidneys. Usually the kidneys filter blood and remove waste produced by the activities of the body. When the kidneys no longer function correctly, the waste produced by the body cannot be removed by the affected kidneys. The
build-up of these toxins can be fatal if you are not treated.
One way of getting rid of the waste is to connect you to an artificial kidney machine. This process is called haemodialysis. It involves diverting your blood into an external dialysis machine, where most of the waste is filtered out. The purified blood is then returned to your body.
To achieve adequate dialysis, a minimum blood flow of 300 millilitres of blood (about a cupful) must flow through the dialyser every minute.
Most people need two or three sessions of haemodialysis a week, for an average of four hours each session.
In order for you to be connected to the dialysis machine, we need access to your bloodstream. The arteriovenous fistula is the best form of access. The fistula is explained in more detail in the next few pages.
What is an arteriovenous (AV) fistula?
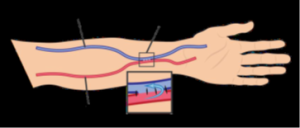
It is an enlargement of a vein. It is formed by joining an artery to a vein under the skin.
Why do I need a fistula and what are the alternatives?
Your consultant will have discussed with you the reasons why you need a fistula.
The three main ways to access a person’s bloodstream for long term dialysis are:
- An arteriovenous fistula
- A haemodialysis catheter
- An arteriovenous graft
If your blood vessels are too small for a fistula, too far apart or affected in any way, the graft is then the best choice. The catheter is used for people who have problems with blood vessels in their arms and legs. Without access to your bloodstream, you cannot have haemodialysis.
Each person is assessed for the option best suited to them.
Where is the fistula placed?
It is usually put in the arm. The ideal site is in the wrist joint area just behind the thumb (please see figure 1). It can also be created in the forearm and in the upper arm above the elbow joint.
How is the AV fistula created?
The AV fistula is created by your renal consultant or a vascular surgeon in an operating theatre. The operation can be carried out using a local anaesthetic (the area is numbed) or general anaesthetic (where you will be asleep). This will depend on your general health at the time.
The surgeon will:
- Make a small cut of about six centimetres long (two inches) in the skin where the fistula is to be created.
- Make another cut (six centimetres long) on the side of the artery and vein to be used.
- Stitch the artery and vein together to leave an opening in the middle. The connection between the two blood vessels is called the AV fistula.
A larger volume of blood can now flow from the artery directly into the vein without going to the hand first. It is this shortcut that makes the fistula buzz and vibrate when touched. This is also known as the buzz or the thrill.
The surgeon will test your blood flow while you are still in theatre.
After your operation, you will be able to feel or listen to the sound of the fistula. This means that it is already working.
How long does the operation take?
It takes about an hour.
How long does the fistula last?
This will depend on the individual’s general health. Generally, a trouble-free fistula can last up to 10 years. Some will work for up to 20 years.
What happens when the fistula wears out?
No-one can guarantee how well the fistula will perform. If the fistula fails, there are opportunities for another to be formed. However, this will depend on how good the other blood vessels are in the arms. Another fistula can sometimes be created in the same arm, higher up, or in the other arm.
If all fails, there is the possibility of using a long-term catheter. This catheter is inserted into a vein in the neck. You can get more details on this type of access from the Renal Unit.
When can the AV fistula be used for dialysis?
After a period of eight to 12 weeks, the fistula will be ready to use for dialysis. This means that the fistula will have grown in size to allow needles to be put in.
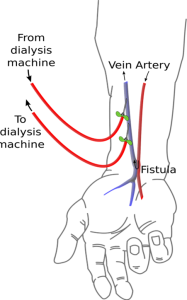
When you come for your dialysis treatment, the nurse looking after you will assess the fistula and will use specially manufactured needles to insert into the fistula. We will usually insert two needles as this will give you the best possible dialysis treatment.
Occasionally, the nurse may insert only one needle to begin with if you have another way of accessing your bloodstream such as a long term catheter. If the nurse does this, they will explain this to you in more detail.
At first we will use small needles and monitor your fistula every session. Over a period of about six weeks, we will increase the size of the needles. This will allow the fistula to reach an ideal size and give a good blood flow, which will provide you with good dialysis treatment.
How do I care for the fistula?
Once the fistula has been put in, you will need to care for it to make sure that it works well and will last. The renal nurse will explain to you how to check and care for your fistula.
The important thing is that the buzz must be strong, meaning that the blood flow is good. The renal staff will explain more about this to you before your operation.
Here are some tips to help you look after your fistula:
Do:
- Feel the buzz of the fistula as often as you can, especially before bedtime and after waking up. This will tell you how strong the blood flow is.
- Listen to the fistula by placing it next to your ear. If you cannot hear or feel the buzz, contact the Renal Unit straight away. The earlier you tell us, the more chance there is of it being ‘rescued’.
- Wear the padded dressing that we give you after the operation for at least one week until you have seen the renal vascular access nurse. This will protect the fistula from knocks.
- Wear gloves in cold weather to keep your hand warm. This will increase circulation and will reduce the risk of your fingertips getting cold. Make sure the gloves are not tight around your wrist.
- Wear gloves when you are gardening. They will protect you from scratches and cuts which may cause an infection.
- Always use a protective leather pad or thick cloth on the fistula arm if you are working in hazardous areas.
- Carry packs of gauze dressing and a roll of tape with you at all times, just in case the fistula bleeds after a dialysis session.
- Exercise the arm that has the fistula as advised by the Renal Unit staff.
- Wear the alert wrist band that the renal vascular access nurse will give you on your wrist to inform others you have a fistula.
- Contact the Renal Unit if you have any questions about the fistula.
Do not :
- Wear tight sleeves above the fistula. This may restrict the blood flow to the fistula. If your blood flow is restricted for a long time, it can cause the fistula to clot.
- Lift heavy objects or bags with the arm that has the fistula in it.
- Allow anyone to take blood or put needles in your fistula except Renal Unit staff.
- Allow anyone to take your blood pressure on the arm that has the fistula in it.
- Keep your arm raised above your head for long periods e.g. working on ceilings. This will reduce the blood flow to the fistula and may cause clotting.
What risks are associated with the fistula?
As with all operations, there are certain risks involved. We aim to reduce these risks as much as possible.
Here are some of the risks of having a fistula:
- Temporary and/or partial loss of feeling in the fingers.
- The hand with the fistula may feel colder than the other one.
- The skin colour of the hand or fingertips may be paler.
- The blood vessels in the fistula arm will increase in size over a period of time.
- Occasionally, you may feel sharp pains in the fistula. If this persists, please tell your renal nurse.
- The fistula may clot and may become unusable for dialysis.
- The fistula may bleed a lot after the needles are taken out.
- The fistula can swell up and cause slowing down of the blood flow in it.
- Very rarely, a fistula may become infected and could cause septicaemia, a blood stream infection that can spread to your heart, other joints or your brain.
The haemodialysis staff will always do their best to ensure that your fistula receives the best care and attention. Our practices are based upon research, training and many years of experience.
Advice in an emergency situation
If the fistula flow is slower or the buzz is weak or has stopped:
If at any time you feel that there is a change in the fistula buzz, this may indicate that the blood flow is reduced. This is why the buzz becomes weaker.
What should I do?
- Call the Renal Unit immediately.
- Wrap your arm in a warm towel.
- Be prepared to come to hospital soon after the call.
Bleeding emergency from fistula or graft
Occasionally, a fistula may bleed a little after the plaster is removed at home. If this happens, it should stop quickly when pressure is applied.
However, although it is a very rare occurrence, you should be aware of the actions to take if profuse bleeding occurs from a fistula or graft site unexpectedly between dialysis sessions.
This is a medical emergency
- Seek help urgently from anyone who is around. The blood flow can be fast and make you feel faint, so do not delay in alerting others.
- Dial 999 and report “excessive bleeding from a dialysis fistula”.
- Apply firm pressure over the bleeding site, use gauze and two fingers, or a bottle top or similar can help localise pressure over the bleeding site.
The pictures overleaf will guide you on how to apply pressure to the bleeding site.


- Do not use too large a dressing. For example, a towel may stop you applying enough pressure in the right place.
- If the bleeding is not controlled by you pressing on it, lie down and ask someone to help by supporting your arm over your head.
- Check you are pressing in the right place.
- Stay calm. Bleeding can usually be stopped with enough pressure in the right place. It may take more pressure than usual if the bleeding is not easily controlled.
- If the bleeding stops before help arrives, it is important that your fistula is still checked urgently as bleeding should not happen between dialysis sessions.
- You should attend hospital so your fistula can be checked by a fistula surgeon.
- Ask the staff in the Emergency Department to contact your Renal Unit.
- Please be aware that this is a rare occurrence, but it’s important that you and your family know how to act if it should occur. Being aware of signs of complications and reporting these promptly should ensure that you do not experience a bleeding emergency.
If you have any questions, or if there is anything you do not understand, please contact the Russells Hall Hospital switchboard number on 01384 456111 and ask for the relevant department who issued this leaflet.
If you have any feedback on this patient information leaflet please email dgft.patient.information@nhs.net
This leaflet can be made available in large print, audio version and in other languages, please call 0800 073 0510.
Originator: Bobbie Bedford. Date reviewed: August 2023. Next review due: May 2026. Version: 7. DGH ref: DGH/PIL/01245.
