Ophthalmology
Glaucoma drainage surgery Baerveldt tube-shunt implant
Patient Information Leaflet
Introduction
This leaflet has been written to help you understand more about the surgery for glaucoma, known as a Baerveldt tube-shunt implant. It explains what the operation is, the benefits and risks of it, and what you should do afterwards.
This information is designed to help you decide whether you would like this surgery, and to make you aware what to expect when you come to hospital.
What is glaucoma?
Glaucoma is an eye disease that can affect sight, usually due to a build-up of pressure within the eye. This eye pressure is known as intraocular pressure (IOP). If it is not treated or if treatment is delayed, it can cause blindness.
A fluid (called aqueous humour) is produced inside the eye. This fluid is needed to
- Provide nutrients to the front of the eye, especially the cornea and lens.
- Remove waste products from the eye.
The fluid drains mainly through a structure called the trabecular meshwork. This meshwork lies inside the eye in the angle where the cornea meets the iris. The normal pressure in the eye is between 10 and 21 millimetres of mercury (mmHg). If for any reason the fluid flow is blocked and cannot normally get out, the pressure can rise and glaucoma may occur.
What treatment options and alternatives are there?
There are various treatment options including tablets, eye drops, laser treatment and drainage surgery, which includes; trabeculotomy, iStent, trabeculectomy and glaucoma tube surgery. Your consultant will discuss all the possible options with you and you can decide which option you prefer. Eye drops and selective laser trabeculoplasty (SLT) are by far the most commonly used initial treatments.
You do not have to have treatment – it is ultimately your decision. However, if glaucoma is not treated, it may eventually cause blindness. Please note that almost all glaucoma treatments and procedures, including laser treatments, are used to control / slow down glaucoma and usually not to regain lost vision.
Once vision is lost from glaucoma, you cannot get it back. All treatment for glaucoma is aimed at slowing down the rate of progression of glaucoma and to reduce the risk of complete blindness during your lifetime.
What is a tube-shunt?
Tube-shunts are devices that are used to reduce the intraocular pressure (IOP) in glaucoma by draining the fluid (aqueous humour) from inside the eye. Reducing the pressure on the optic nerve in this way may prevent further damage and further loss of vision from glaucoma.
What is tube-shunt implant surgery?
It is an operation to implant a tube-shunt into your eye. A tube-shunt is a silicon tube that has a diameter outside of 0.64mm, so it is very small.
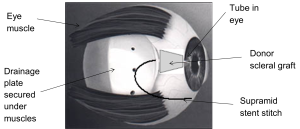
During the operation, one end of the tube is securely inserted into the front part of the eye. The other end is connected to a white silicon plate that rests on the surface of the eye (sclera), underneath the eye lid. This plate acts like a reservoir for the fluid from inside the eye to be drained away.

A membrane called the conjunctiva covers the front of the eye and lines the inside of the eyelids. It covers the silicon plate and absorbs the fluid that collects in it. As the fluid can now drain through the newly created drainage channel, your eye pressure will be reduced.
When the tube-shunt is first put in, the eye surgeon will partially close it with a stitch called a Supramid stent stitch. This helps to prevent too much fluid coming out of the eye which would cause the eye pressure to be too low.
As the tube-shunt settles in, this stitch can be adjusted to either let more or less fluid out, depending on the pressure of fluid in your eye.
The glaucoma tube-shunt is going to stay in the eye for the rest of the person’s life, so we need to cover the portion of the tube outside the eye. This prevents the tube from moving and becoming exposed. To do this, we can either use a donor scleral patch graft (see figure 2) or a Tutoplast scleral patch graft.
What is a donor scleral patch graft?
It is a piece of sclera (the white tissue of the eye) and it is attached to the eye using stitches.
The tissue is obtained from deceased people who donated their organs for medical use after death. It is obtained from the Human Tissue Bank in the UK. The donors have been screened for any diseases that can be spread from one person to another, except for
- Prion infection which could cause Creutzfeldt-Jakob disease (CJD).
- Spongiform encephalopathy.
These diseases cannot be detected by the normal screening procedures. However, it is extremely rare for people to get an infection from receiving donor tissue. Please discuss this with our glaucoma team if you have any concerns about this.
What is a Tutoplast scleral patch graft?
It is a piece of human tissue called collagen that has been sterilised and preserved using a method called the Tutoplast process, making it safe to use as a graft. Again, this tissue is obtained from deceased people who donated their organs for medical use after death.
Why is this operation recommended?
Glaucoma tube-shunt implant surgery is a complex procedure that is normally recommended for patients with specific types of glaucoma, such as
- Complex secondary glaucoma. Secondary glaucoma is where the cause of increased eye pressure can be linked to other eye conditions, operations, injuries or medications.
- Advanced glaucoma.
- Glaucoma where eye pressure is not controlled, even on maximum glaucoma medications, or has not responded to other types of glaucoma treatment.
It is also recommended when conventional glaucoma drainage surgery (trabeculectomy) is unlikely to be successful and when previous glaucoma drainage surgery has failed.
It is used to treat difficult and uncontrollable glaucoma, not to improve vision. In glaucoma, vision or visual field which is already lost cannot be recovered or restored.
What are the benefits?
This operation is not aimed at improving your vision or to cure glaucoma, but aims to slow down further loss of your sight from glaucoma damage. The goal is to reduce your risk of blindness from glaucoma in your lifetime.
How successful is tube-shunt implant surgery?
The tube-shunt operation is generally a very successful operation for glaucoma that has not responded to other types of glaucoma treatment. Research has shown that eye pressure is reduced in about 80 per cent of patients (eight out of every 10 patients), followed up one year after surgery.
The success rates usually go down with time. However, if needed, the operation can be repeated or another treatment can be offered. Some patients may also need to use one or more glaucoma eye drop medications to maintain a satisfactory eye pressure level. If the tube-shunt surgery fails, other surgical or laser procedures may be needed.
What are the risks?
As with all surgery, this operation carries some risks and complications. It is important that we tell you about these risks so you have the information you need to make a decision about the operation.
Complications that can occur in some patients
Eye pressure could become too low when the tube-shunt starts working. The medical name of this is hypotony.
If this happens, it may be necessary to inject a ‘jelly-like’ substance (known as viscoelastics) into the front part of your eye, to maintain eye pressure until it stabilises.
If your eye pressure remains too low, you may need to have a procedure to adjust the Supramid stent stitch on the tube-shunt to let less fluid out. This prevents complications from low eye pressure.
Other risks of the operation include infection, reduced sight or a loss of sight, bleeding inside the eye, double vision, a droopy eyelid, pain, haziness in the cornea and very rarely, retinal detachment. Cataract formation may be increased by this surgery and this may cause reduced vision.
If you have a general anaesthetic, this can cause serious problems such as an allergic reaction, but these are very rare. If you have any worries about this, you can discuss them at your meeting before your operation (health assessment), or with the anaesthetist before your operation.
What happens before the operation?
You will be given information on the surgery and an informed consent will be taken. You should continue to take any eye drops and tablets for your glaucoma as prescribed until the time of your surgery, unless you are told not to use them. You may be asked to use a new eye drop four times a day, up to four weeks prior, in the eye that will be having surgery.
If you are taking any blood thinning tablets (such as warfarin or aspirin) they may increase the risk of bleeding during the operation. You should discuss this with your glaucoma team. They may advise you to stop them for a week before surgery, if this will not affect your general health. You may discuss this with your GP and if it is advisable to stop, when it is safe enough to do so.
You will be given instructions about eating and drinking before the operation in your operation appointment letter.
What happens during the operation?
The doctor will explain the treatment to you and discuss any concerns or questions you may have with you. If you are happy to proceed with the treatment, your consent will be reconfirmed.
You will usually be given a general anaesthetic for the operation. This means you will be asleep during the procedure. Your anaesthetist will discuss this with you before the operation.
How long does it take?
The operation usually takes about three hours to perform.
What happens after the operation?
After the operation, you will be taken to the recovery area where you will wake up. In the recovery area, nursing staff will look after you, checking your blood pressure and pulse, and giving you pain relief medication, if needed.
Immediately after your operation, your eye will be covered by an eye pad and protective plastic shield.
Once the nurses are happy that you have completely recovered from the operation and general anaesthetic, you can go home. We will give you all the medications you need. The team will make an appointment for you to be reviewed the next morning in the glaucoma clinic.
What can I expect after tube-shunt surgery?
The eye pad and shield will be taken off in the glaucoma clinic the morning after your operation. You will have to take steroid tablets for three weeks, on gradually decreasing doses. You will also need to use a few eye drop medications. If you feel you cannot take steroid tablets for any reason, please talk to your glaucoma team.
Your eye will be a bit gritty and sore for at least a few days. Your eye may feel sore for a few weeks. After your eye has settled down, the tube is usually not visible. However, you may be able to feel the device under your upper eyelid. As the tube remains inside your eye, try not to rub your eyes as this might cause the tube to move and damage other parts of the eye.
What should I look out for at home?
If you have any of the following after trabeculectomy surgery:
- Reduced vision or loss of vision.
- Severe pain that does not go away.
- Any abnormal discharge from your eye, especially if it is increasing.
Please contact the Urgent Referral Clinic team at Russells Hall Hospital Eye Clinic on 01384 456111 ext. 3633.
Follow up appointments
You will need to be closely followed up in the glaucoma clinic in the first three months after the surgery. It is therefore a good idea not to be away or outside the country during this critical period.
In order that we can check your eye, you will need to come to the Eye Clinic after one day, one week, two weeks and later depending on how your eye is recovering.
What happens if my eye pressure rises again after the
tube-shunt operation?
The tube-shunt is partly blocked by the Supramid stent stitch which is used to prevent low eye pressure. If the eye pressure starts to rise again, the stitch can be removed or adjusted to allow more fluid through the tube. This procedure is carried out using a local anaesthetic, so your eye will be numb.
Sometimes, eye pressure is still too high due to a large amount of scar tissue forming over the tube-shunt drainage plate. In this case, we can carry out a procedure to put tiny holes in the scar tissue, using an anti-scarring medication.
Alternatively, we can carry out laser treatment to improve the function of the tube-shunt.
Follow up
Even if your eye pressure has stabilised after tube-shunt surgery, we will still need to see you at the glaucoma clinic for regular monitoring. Your eye pressure could rise again in the future.
Also, it is possible that the position of the tube may need to be adjusted if it moves and becomes too close to the cornea. A cataract may also form, which may require a cataract operation.
Can I find out more?
You can find more information on glaucoma, the risk of blindness from glaucoma, and various treatment options from the following websites:
http://www.glaucoma-association.com/
http://www.glaucoma-association.com/about-glaucoma/what-is-glaucoma
http://www.nei.nih.gov/health/glaucoma/glaucoma_facts.asp
http://www.rnib.org.uk/eyehealth/eyeconditions/eyeconditionsdn/Pages/glaucoma.aspx
http://en.wikipedia.org/wiki/Glaucoma
http://www.nice.org.uk/guidance/cg85/ifp/chapter/About-this-information
https://www.rcophth.ac.uk/patients/glaucoma/
What if I have any problems or questions after reading this leaflet?
If there is anything you do not understand, or you are concerned or worried about any part of the treatment, contact:
The Urgent Referral Clinic team at Russells Hall Hospital Eye Clinic on 01384 456111 ext. 3633.
Eye emergency, out of hours
In case of an eye emergency after the closing hours of the Eye Clinic at Russells Hall Hospital (including weekends and bank holidays), please contact:
Birmingham and Midland Eye Centre on 0121 507 4440
The doctor on call is usually based at the Eye Centre, City Hospital, Dudley Road, Birmingham. They may need to call you back, and if necessary, they will arrange for you to visit them.
Note: the information in this booklet is provided for information only. The information found is not a substitute for professional medical advice or care by a qualified doctor or other health care professional. Always check with your doctor if you have any concerns about your condition or treatment. This is only indicative and general information for the procedure. Individual experiences may vary and all the points may not apply to all patients at all times. Please discuss your individual circumstances with your eye doctor.
Author: Mr Akash Raj, MD, MRCS, DRCOphth, FRCS, FRCOphth consultant ophthalmologist (glaucoma lead)
References: Christakis PG, Kalenak JW, Zurakowski D, Tsai JC, Kammer JA, Harasymowycz PJ and Ahmed II (2011). The Ahmed Versus Baerveldt study: one-year treatment outcomes. Ophthalmology. 118(11):2180-9.
If you have any questions, or if there is anything you do not understand, please contact the Russells Hall Hospital switchboard number on 01384 456111 and ask for the relevant department who issued this leaflet.
If you have any feedback on this patient information leaflet please email dgft.patient.information@nhs.net
This leaflet can be made available in large print, audio version and in other languages, please call 0800 073 0510.
Baerveldt/AR/ST/DP/09 2024 /v4 – review 06 2027 DGH/PIL/01150
