Ophthalmology
Glaucoma drainage surgery (trabeculectomy)
Patient Information Leaflet
Introduction
This leaflet has been written to help you understand more about the surgery for glaucoma known medically as a trabeculectomy. It explains what the operation involves, the benefits and risks of it, and what you should do afterwards.
This information is designed to help you decide whether you would like this surgery and to make you aware of what to expect when you come to hospital.
What is glaucoma?
Glaucoma is an eye disease that can affect sight, usually due to a build-up of pressure within the eye. This eye pressure is known as intraocular pressure (IOP). If it is not treated or if treatment is delayed, it can cause blindness.
A fluid (called aqueous humour) is produced inside the eye. This fluid is needed to:
- Provide nutrients to the front of the eye, especially the cornea and lens.
- Remove waste products from the eye.
The fluid drains mainly through a structure called the trabecular meshwork. This meshwork lies inside the eye in the angle where the cornea meets the iris. The normal pressure in the eye is between 10 and 21 millimetres of mercury (mmHg). If, for any reason, the fluid flow is blocked and cannot get out normally, the pressure can rise and glaucoma may occur.
What treatment options and alternatives are there?
There are various treatment options including tablets, eye drops, laser treatment and drainage surgery, which includes trabeculotomy, iStent, trabeculectomy and glaucoma tube surgery. Your consultant will discuss all of the possible options with you and you can decide which option you prefer. Eye drops and laser trabeculoplasty are by far the most commonly used initial treatments.
You do not have to have treatment – it is ultimately your decision. However, if glaucoma is not treated, it may eventually cause blindness.
Please note that almost all glaucoma treatments and procedures, including laser treatments, are used to control / slow down glaucoma and not to improve your vision. Once vision is lost from glaucoma, you cannot get it back. All treatment for glaucoma is aimed at slowing down the rate of progression of glaucoma, to reduce the risk of complete blindness during your lifetime.
What is a trabeculectomy?
It is an operation to create an alternative secure drainage channel under the superficial layers of your eye, to help aqueous fluid (the natural fluid of the eye) drain from your eye. It therefore creates a bypass for the blocked natural drain in your eye. Your eye pressure will be reduced because fluid can now drain through the newly created drainage channel.
The drainage occurs inside those superficial layers of your eye, and you should not be able to see or feel this.
Why is this operation recommended?
It is recommended for patients who have glaucoma where it continues to get worse or progresses despite using eye drops and / or having had laser treatment.
What are the benefits?
This operation will not improve your vision or cure glaucoma, but it aims to control or slow down further visual loss from glaucoma damage. The goal is to reduce the risk of blindness from glaucoma in your lifetime.
How is a trabeculectomy operation performed?
During the operation, a tiny opening is made in the white of your eye (the sclera), underneath the top eyelid, to form a new drainage channel. This allows the eye fluid to drain through the new opening into a reservoir, called a bleb, and then to be absorbed by the body.
The bleb is underneath the thin transparent layer covering the white of your eye (known as the conjunctiva). This is on the surface of your eye, underneath the top eyelid (see figure 1). Trabeculectomy surgery can be carried out using either a local anaesthetic or a general anaesthetic. Your consultant will discuss this with you.
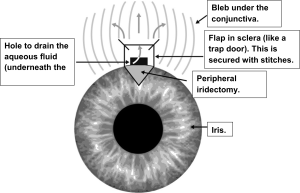
Figure 1 shows where the new drainage channel is made.
How successful is trabeculectomy surgery at lowering intraocular pressure (IOP)?
Research on the success of trabeculectomy surgery shows it is dependent upon many factors. Where the success of trabeculectomy surgery is based on a patient’s IOP, eye pressure is reduced by at least one third in 66 per cent of patients followed up one year after surgery. Our audits (Mr Raj’s and Mr Elahi’s) show better success rate in Dudley as compared to the National Trabeculectomy Audit results. Of our patients, 86.1 per cent achieved an eye pressure under 21mmHg and stabilisation of visual fields following surgery as compared to 80 per cent in the national standards at 24 months after surgery.
The success rates usually go down with time. However, if needed, the operation can be repeated or other treatments can be offered. About one third of patients may need to use one or more glaucoma eye drops to maintain a satisfactory eye pressure.
There are a few factors that can reduce the success of trabeculectomy surgery. These are people who:
- Are of a younger age.
- Are of Asian or Afro-Caribbean heritage.
- Have uveitis, which is inflammation within the eye.
- Have very high pressure in eye.
- Have had a previous glaucoma procedure that failed.
- Have had eye surgery before.
- Have had a severe eye injury.
- Have rubeotic glaucoma – a condition where there are abnormal blood vessels on the iris.
- Have an ‘over efficient’ natural healing process.
- Have diabetes.
If the trabeculectomy surgery fails, you may need to have more surgical or laser procedures.
What are the risks?
As with all surgery, this operation carries some risks and complications. It is important that we tell you about these risks so that you have the information you need to make a decision about the operation.
These complications can happen during surgery, shortly after surgery or many months or years after surgery.
Complications that can occur include:
- Bleeding – a serious but rare complication from this surgery. It can lead to loss of vision and even blindness, although this is very rare.
- An infection inside the eye – this can be very serious and can also cause loss of vision or blindness. This is also rare (about one to two people out of 100 may get this).
- After the operation, your eye pressure may be too high or too low. If this happens, you may need more treatment, a minor procedure to adjust it, or sometimes more surgery.
- Your eye may be inflamed for a prolonged period after surgery. This is usually for up to three months, but can be longer depending on individual circumstances.
- Swelling in the retina – this can affect your vision, but this is mostly treatable.
- Some people with very advanced glaucoma may experience a permanent complete loss of vision and their visual field. This is called a ‘wipe out’ phenomenon and is quite rare.
- If you have a general anaesthetic, this can cause serious problems such as an allergic reaction, but these are very rare. If you have any worries about this, you can discuss them at your meeting before your operation (health assessment) or with the anaesthetist before your operation.
- Some patients are aware of the drainage bleb under their upper eyelid, or some have a slight drooping of the eyelid, but this usually settles down. As your eye settles down and heals, you may need to change your glasses to get your best vision.
- About 10 per cent of patients (one person out of every 10) notice that their vision is reduced by one line on the eye chart a year after the operation.
- Cataract formation may be increased by trabeculectomy surgery and this may cause reduced vision. There may be a need for subsequent cataract surgery (usually more than six to 12 months after the glaucoma surgery).
The use of anti-scarring medications
The main reason trabeculectomy surgery can fail is that the newly-created drainage site can scar and heal up due to your own body’s natural tendency to heal. Some people are more likely to get this than others.
There are medications that can help prevent scar tissue formation. The medical name for these is antimetabolites. If we are concerned that you may get excess scarring, we will recommend that these are used to limit scarring and therefore improve the success rate of the operation. The most commonly used antimetabolites are mitomycin C (MMC) and
5-Fluorouracil (5FU). These can be used at the time of surgery or afterwards.
What happens before the operation?
You should continue any eye drops and tablets for your glaucoma as prescribed, unless specifically directed otherwise. You may be asked to use a new eye drop four times a day, up to four weeks prior, in the eye that will be having surgery.
If you are taking any blood-thinning tablets such as warfarin or aspirin, they might increase the risk of bleeding during the operation. You should discuss this with your glaucoma team or your GP. They may advise you to stop them for a week before your surgery if it is safe to do so and will not affect your general health.
What happens during the operation?
We will give a local anaesthetic to your eye a few minutes before the start of the operation.
To do this, we will put numbing drops into your eye and, when your eye is numb, we will inject the anaesthetic into the tissue around your eye. You may feel pressure when we do this, but it is not usually painful. This makes the eye numb and usually blurred as well. If you are having a general anaesthetic, we will give you a separate leaflet about this.
You will need to lie on your back for the operation. A clip will be used to keep your eye open. You may see light and shadow, but you will not see the surgery happening. The operation may also be done under general anaesthetic (this means you will be asleep).
How long does it take?
It usually takes between 70 and 100 minutes to complete the operation.
What happens after the operation?
Immediately after your operation, your eye will be covered by an eye pad and a protective plastic shield. Your eye may be uncomfortable and you may have some pain and tenderness after the operation. We will give you advice about pain relief. You do not usually need to put eye drops into your operated eye until the day after surgery. However, if you usually use eye drops in your other eye, you must continue to use these as normal.
The morning after your operation, you will need to come back to the hospital for the eye pad and protective eye shield to be removed. Your eye will be cleaned and examined, and you will be given eye drops for the operated eye. The eye drops you will need to use in your operated eye will be different from the drops that you used before your operation (previous drops should be stopped after the surgery).
You will need to use these drops for approximately three months after your operation. When you come for follow up visits (usually three visits – one day after surgery, one week after surgery and two weeks after surgery) to the glaucoma clinic, we may need to change the eye drops that you are using. We will discuss this with you. If you are running out of the eye drops, you must obtain a repeat prescription for them from your GP.
You may need to take about two weeks off work after the operation. During the first two weeks after the operation, we advise you not to put any pressure on the eye, and not to bend or lift heavy items. You will need to wear your eye shield over the operated eye at night (every night) for approximately two weeks.
What should I look out for at home?
If you have any of the following after a trabeculectomy surgery:
- Reduced vision or loss of vision.
- Severe pain that does not go away.
- Any abnormal discharge from your eye, especially if it is increasing.
Please contact the Urgent Referral Clinic team at Russells Hall Hospital Eye Clinic on 01384 456111 ext. 3633.
Follow up visits
You will need to come for frequent follow up visits after the operation. The success of trabeculectomy surgery depends on how you are healing. Also, your IOP can change a great deal in the first few weeks after surgery.
Therefore, in order for us to check your eye, you will need to come to the Eye Clinic after one day, one week and later depending on your particular condition.
At these visits, we may need to make adjustments to maximise the success of your surgery. These include changing your eye drops, adjusting or removing stitches, and possibly having anti-scarring injections. It is very important that you come for all of your clinic appointments and use your eye drops as prescribed. It is a good idea not to be away or outside the country during these critical three months after surgery.
Can I find out more?
You can find more information on glaucoma, on the risk of blindness from glaucoma and various treatment options from the following websites:
http://www.glaucoma-association.com/
http://www.glaucoma-association.com/about-glaucoma/what-is-glaucoma
http://www.nei.nih.gov/health/glaucoma/glaucoma_facts.asp
http://www.rnib.org.uk/eyehealth/eyeconditions/eyeconditionsdn/Pages/glaucoma.aspx
http://en.wikipedia.org/wiki/Glaucoma
http://www.nice.org.uk/guidance/cg85/ifp/chapter/About-this-information
https://www.rcophth.ac.uk/patients/glaucoma/
What if I have any problems or questions after reading this leaflet?
Please contact the Urgent Referral Clinic team at Russells Hall Hospital Eye Clinic on 01384 456111 ext. 3633 (9am to 4.30pm, Monday to Friday).
Eye emergency, out of hours
In case of an eye emergency after the closing hours of the Eye Clinic at Russells Hall Hospital (including weekends and bank holidays), please contact:
Birmingham and Midland Eye Centre on 0121 507 4440
The doctor on call is usually based at the Eye Centre, City Hospital, Dudley Road, Birmingham. They may need to call you back, and if necessary, they will arrange for you to visit them.
Note: the information in this booklet is provided for information only. The information found is not a substitute for professional medical advice or care by a qualified doctor or other health care professional. Always check with your doctor if you have any concerns about your condition or treatment. This is only indicative and general information for the procedure. Individual experiences may vary and all the points may not apply to all patients at all times. Please discuss your individual circumstances with your eye doctor.
Author: Mr Akash Raj, MD, MRCS, DRCOphth, FRCS, FRCOphth, Consultant ophthalmologist (glaucoma lead)
References
Edmunds B, Thompson JR, Salmon JF and Wormald RP (2001). The National Survey of Trabeculectomy. II. Variations in operative technique and outcome. Eye (Lond). 15(Pt 4):441-8.
Zahid S, Musch DC, Niziol LM, Lichter PR and Collaborative Initial Glaucoma Treatment Study Group (2013). Risk of endophthalmitis and other long-term complications of trabeculectomy in the Collaborative Initial Glaucoma Treatment Study (CIGTS). Am J Ophthalmol. 155(4):674-680, 680.e1.
If you have any questions, or if there is anything you do not understand, please contact the Russells Hall Hospital switchboard number on 01384 456111 and ask for the relevant department who issued this leaflet.
If you have any feedback on this patient information leaflet please email dgft.patient.information@nhs.net
This leaflet can be made available in large print, audio version and in other languages, please call 0800 073 0510.
Trab/AR/ST/04.02 2025/v4– review 11.2027 – DGH ref.: DGH/PIL/01148
