Acute Medicine Department
Having a lumbar puncture
Patient Information Leaflet
Introduction
This leaflet is for adults who are going to have a lumbar puncture. It explains:
• What the lumbar puncture involves.
• Why it is done and the possible risks.
• What will happen after you have had the lumbar puncture.
What is a lumbar puncture?
This procedure (sometimes called a ‘spinal tap’) is used to obtain a sample of the fluid that surrounds the brain and spinal cord called the cerebrospinal fluid (CSF).
Why do I need a lumbar puncture?
A lumbar puncture may be done for various reasons. The most common reason is to remove a small amount of CSF for testing. This can help in the diagnosis of various disorders.
Depending on your symptoms, the fluid may be tested for red and white blood cells, protein, glucose (sugar), to see whether bacteria, viruses, or abnormal cells are present, and possibly for other specialist tests. The clarity and colour of the fluid are also checked and, when necessary, CSF pressure will be measured to see if it is within the normal range.
Excess CSF may also be removed in people who have an overproduction or decreased absorption of the fluid.
What are the risks?
Headache
This is the most common side effect and is due to decreased pressure of the CSF following removal of the fluid. It can start a few hours to two days after the procedure, and it can last for a few days. It is caused by fluid being removed and / or the slow leak of spinal fluid through the puncture site into the tissue. It is not dangerous and the leak closes over a few days. The headache may be dull or throbbing, and you may also have a stiff neck and feel nauseous. It can be treated by lying flat and taking pain relief medication such as paracetamol.
Very rarely, the headache can last several weeks or months and will need an injection to seal the lumbar puncture site. Drinking plenty of fluid, caffeine and eating salted snacks can help to reduce the risk of headache. If it does not settle or is severe, let your doctor know.
Back pain
You may experience some back pain after the procedure from where the local anaesthetic injection and lumbar puncture needle was inserted. You may also have some bruising. If you have any back pain after the lumbar puncture, you can treat this with pain relief medication such as paracetamol.
Tingling in your legs
Nerve damage after a lumbar puncture is extremely rare (one in 1000). Sometimes during the procedure, the nerves that float in the fluid can touch the sides of the needle, causing them to be stimulated. When this happens, it gives a feeling of tingling down the leg that lasts for a few seconds.
Infection / fever
This is extremely rare. There is always a risk of infection being introduced, as the needle has to go through the skin. The risk is reduced by cleaning the skin and using aseptic techniques and hygiene practices. If you get symptoms of infection, like a fever, you must contact your doctor immediately.
Other complications
In very rare cases, a blood clot may form around the lumbar puncture site or around the brain. This would be very serious and may require surgery to treat it. There have also been extremely rare reports of persistent back pain, numbness and tingling of the leg, hearing loss and double vision following a lumbar puncture.
Serious harm due to complications such as these occur in less than one in 10,000 lumbar punctures. The clinicians looking after you will have weighed up the risks of the procedure against the potential benefits and will always ensure that the procedure is only undertaken if it is absolutely necessary.
What happens before a lumbar puncture?
The clinician looking after you will speak to you about the procedure and answer any questions you may have. After this, a consent form will need to be signed by yourself. Please make sure you empty your bladder before the procedure so that you are not uncomfortable during it.
Do not drive on the day of the lumbar puncture – please ensure that you have someone who can drive you back (if you are going home on this day).
What happens during the lumbar puncture?
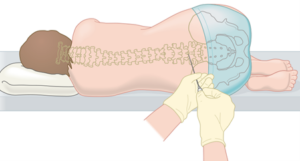
Lumbar puncture needle being placed. Illustration used with kind permission of Lymphoma Action.
The lumbar puncture usually takes around 15 to 20 minutes. This is what happens:
- You will either be asked to lie on your side with your knees curled up to your stomach, or you will be asked to sit on the side of the bed, bending forward. A nurse may help you tuck your head towards your chest.
- Your lower back is washed with a disinfectant to clean the skin.
- You will then be given a local anaesthetic injection to numb the area. This may sting for a few seconds.
- The clinician will carefully put a needle into a space in the lower back, below where the spinal cord ends. You will need to hold very still so that the needle does not move. You may feel some pushing as the needle enters your back, please tell the team if you feel pain. Try not to hold your breath or tighten up your body too much as this can cause CSF pressure readings to be falsely elevated.
- A sample of your spinal fluid is then taken and will be sent to the laboratory for testing.
- A small dressing will then be put on your back.
- You will be asked to lie flat for an hour after the lumbar puncture – this reduces the chance of developing a headache.
What if it is unsuccessful?
Lumbar punctures are usually successful, but sometimes it is not easy for the clinician to find the exact place where the needle should be inserted.
This is more likely in people who have severe arthritis of the spine, have an abnormally shaped spine, or are overweight.
If this happens, the person doing the lumbar puncture may call another clinician to help, but in some cases the procedure has to be stopped. If this occurs, the team will talk to you about the plan following this. Sometimes the team may need to do more than one lumbar puncture to get the information they need.
What happens after a lumbar puncture?
Some people get a headache after a lumbar puncture. This is because, after the procedure, the pressure reduces slightly around the brain. The headache usually goes away after about 24 to 48 hours. You can have paracetamol if you need it and if you are able to take it, so ask the nurse who is looking after you. We advise you to keep yourself well hydrated to try to prevent this, and you can drink caffeine to help.
The dressing from the lumbar puncture can be removed the following day. You can have a shower after six hours providing you feel well enough and do not have a low pressure headache.
The results will be given to you by the team when they are available. Some results, such as pressure measurements and white cell count, will be available quickly. Other results will take longer due to the time needed for analysis in the laboratory. The team looking after you should explain how long the results will take in your case.
Symptoms to report
Please contact your doctor if you have any of the following symptoms while in hospital or after you are sent home:
- Arm or leg weakness or numbness.
- New incontinence or constipation.
- A headache that does not resolve on lying flat.
- A high temperature (38ºC or above).
- Sweats.
- Confusion.
- Strong aversion to bright light.
If you have any concerns after you have been discharged, during the hours of 8am – 7pm, Monday to Sunday, you can contact the same day emergency care (SDEC) – ambulatory emergency care (AEC) front desk on 01384 456111 ext 1815 and ask for the nurse in charge or registrar.
Originator: Jennifer Novy Date reviewed: August 2025 Next review due: May 2028 Version: 1 DGH ref: DGH/PIL/02165
