Radiology Department
Hickman line insertion
Patient Information Leaflet
Introduction
This leaflet explains what a Hickman line is, how it is inserted into the body, and why your doctor has recommended this for you. If you have any questions or concerns, please contact the Interventional Radiology (IR) Department (details at the end of this leaflet).
What is a Hickman line?
A Hickman line is a long, flexible plastic tube that is inserted underneath the chest wall skin and into the large vein draining into the heart (see figure 1). A Hickman line is a type of tunnelled central line. 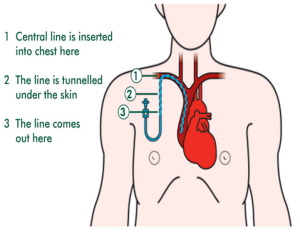
The space in the middle of the tube is called the lumen. Hickman lines can have one, two or three lumens. These allow different medications to be given at the same time, although the external diameter is the same.
Your interventional radiologist will decide how many lumens your line needs.
Part of your Hickman line tube remains outside of the skin. This is so that nurses can use the line to give medications or take blood samples. Usually, the external part of the line can be hidden by clothes (or a bra) so that people will not know that you have a line in place.
How a Hickman line is inserted
It is done by a doctor called an interventional radiologist (anaesthetic doctors are also involved in providing this procedure). It is a minor surgical procedure, and it is done in the IR theatre under local anaesthetic (you will be awake, but you will only feel mild discomfort).
You need to lie flat on the X-ray table for 30 to 40 minutes for the procedure.
Your skin will be cleaned with antiseptic and you will be covered with sterile drapes. Then, you will be given some local anaesthetic to numb the area.
Once the skin is numb, two small (4mm) cuts are made. One will be made on the chest wall where the line will come out, and the second will be made in the neck or around the collarbone where the line goes into the vein. There is a cuff which is used to fix the line under your skin between the insertion and exit sites. It also acts as a barrier against infection entering your body at this point.
The procedure is done using ultrasound (to help identify a suitable large vein) and a special X-ray machine (to check that the line tip is in the correct place). These machines make the procedure very safe and avoid the need for large cuts.
The benefits of having a Hickman line
It is a reliable way for us to give intravenous (directly into a vein) medicines, nutrients, such as total parenteral nutrition (TPN), or to take blood samples. Having a Hickman line means you avoid having a new needle puncture every time you need treatment or a blood test. The Hickman line is meant to remain in place for a long time (months to years), so it can be used throughout your treatment.
Doctors recommend a Hickman line for patients who regularly have chemotherapy, long term antibiotics or TPN. Some medications need to be given directly into a large vein rather than a small vein in the hand or arm. This is to prevent irritation.
The risks of having a Hickman line
Serious risks and complications of having a Hickman line inserted are very rare. However, as with any procedure, there are some risks and complications which you should be aware of:
- The insertion procedure will be done in sterile conditions. It is very important that the Hickman line is kept clean; otherwise, infection can get directly into the blood stream. This would need treatment with antibiotics and, often, the line would need to be removed.
- Lumen blockage. Your line needs regular care to keep it working properly. If it is not looked after, then one or more of the lumens can become blocked and stop working. If the line gets blocked, or breaks and does not work, it will need to be replaced.
- Hickman line insertion requires at least two small cuts in the skin. These will heal as small scars.
- There is a small risk of bleeding or bruising at the insertion site, but this normally resolves by itself.
- The top of the lung is near the puncture site. Very rarely, this can get pierced during the procedure, which may cause some air to leak into the space between the lung and your ribcage (pneumothorax). This is extremely rare, but can be easily treated by inserting a chest drain.
The radiologist will discuss the possible risks with you before you have the procedure. Please ask them if you have any concerns or would like more information.
Will you feel any pain?
A Hickman line is a minor procedure for most patients. It is usually done using local anaesthetic to numb the skin in the neck and chest. Because you are awake during the procedure, you can communicate directly with the staff. There will be a nurse monitoring you throughout the procedure. The line will be ready to use straight away. Simple painkillers (such as paracetamol) can be used if you are uncomfortable
Are other options available?
A Hickman line is a voluntary procedure. One alternative is to have a temporary line placed every time you have your treatment. This new line needs to be placed and removed each time before you leave hospital. Having new lines placed can be painful (and time consuming).
Also, temporary lines might not be suitable for some medications, and they are not practical if you need infusions over a long period of time.
Another option is to have a peripherally inserted central catheter (PICC) line. PICC lines block more easily than Hickman lines and might cause the vein in your arm to clot. Please talk to your doctors or nurses if you would like more information about these alternatives.
Consent – asking for your consent
We want to involve you in decisions about your care and treatment. If you decide to go ahead, you will be asked to sign a consent form. This states that you agree to have the treatment and that you understand what it involves.
If you would like more information about our consent process, please speak to a member of staff caring for you.
Before your procedure
We will arrange for you to have some simple blood tests. The IR doctors need to see a list of all your medications (tablets, inhalers, creams), so please bring a copy of your current prescriptions with you.
Certain medications, particularly blood thinners, will need to be stopped before your procedure. The IR doctor or nurse will advise you if you need to stop any medicines. These medicines can be restarted after your line insertion, but the IR doctor or nurse will advise you on this.
The day of your procedure
- On the day of your procedure, you may have a light breakfast and drink as normal.
- Please arrive on time to allow time for preparation – an appointment will be sent to you in the post, or you will receive a phone call from our theatre co-ordinator. You will need to get changed into a theatre gown. The IR doctors / nurses will go through your medications with you again, and one of the nurses / radiographers will go through some safety checklists with you.
- You will be asked to sign a consent form, agreeing to go ahead with the procedure. This is another opportunity for you to ask any questions you may have.
After your Hickman line insertion
- After your procedure, you will need to rest in the IR department for 30 minutes. This is to make sure that there are no problems. The IR nurse will let you know when you can eat, drink and mobilise after your procedure. If all of your checks are normal, you can go home.
- You will need a responsible adult to escort you home. We do not recommend you using public transport in case you feel unwell.
- We recommend that you have an adult stay with you overnight.
- Do not drive for 24 hours after the procedure, and do not drive until you feel safe enough to do so.
- Avoid any strenuous exercise or lifting for 48 hours after the procedure.
- Simple painkillers (such as paracetamol) can be useful for any discomfort.
- Continue with your normal medications as usual (unless your IR doctor has told you otherwise).
Taking care of your Hickman line at home
- Showering – use a waterproof dressing over the tubing as this will usually keep it dry during the shower. We will give you some dressings and tell you how to use them. You will generally need a dressing for two weeks after the insertion. Afterwards, you only really need to keep it dry while showering.
- Having a bath – submerging the line under water is not advised, due to the risk of infecting your line. However, having a shallow bath and keeping the line out of the water is fine.
- Sports – we strongly advise you to avoid swimming and also saunas. Otherwise, as long as you are careful, most other activities are fine.
Keeping your Hickman line working
We recommend that each lumen of your Hickman line is flushed once a week to stop it becoming blocked. The plastic bungs on the end of the line should be changed weekly. This will be done on the ward or in the day unit where you receive your treatment. The nurses on the day unit or ward can teach you, a family member or a friend how to flush your line at home, if needed.
Alternatively, a district nurse can be asked to see you at home to change the dressing and flush the line, especially on the weeks that you cannot come to the hospital. Please talk to your nurse specialist on the day unit / ward to arrange this.
How will you know if there is something wrong with your Hickman line?
You need to look for signs of serious infection. If you experience a cold, shivery attack during or after flushing your line, contact the doctor or nurse caring for you immediately. This could be due to an infection in the line. The line is in a large vein close to your heart, so it is important to treat any infection as soon as possible.
You should also contact your doctor or nurse if:
- Your line gets damaged or develops a leak / crack / split.
- You develop any redness, swelling or pain around the line site on the skin.
- You notice your line becoming loose at the skin. We want to avoid the line from falling out.
How is the Hickman line removed?
When you no longer need the Hickman line, it will be removed in the IR department. The doctor doing the procedure will give you all the information you need if any preparation is required.
Removing a Hickman line is usually a very quick procedure, compared to inserting the line. The procedure is performed under local anaesthetic.
Useful sources of information
Macmillan Cancer Support
Contact us
If you have any questions or concerns about this procedure, please contact either of the following:
IR Department: 01384 456111 ext. 3124 (Monday to Friday, 8.30am – 5pm)
Oncology / haematology triage: 01384 456111 ext. 4271 (Monday to Friday, 9am – 5pm) or 01384 456111 ext. 2235 (out of hours)
Community IV team, Brierley Hill Health and Social Care Centre, Venture Way, Brierley Hill, DY5 1RU: 01384 321241 (7 days a week, 8am – 6pm)
If you have any questions, or if there is anything you do not understand, please contact the Russells Hall Hospital switchboard number on 01384 456111 and ask for the relevant department who issued this leaflet.
If you have any feedback on this patient information leaflet please email dgft.patient.information@nhs.net
This leaflet can be made available in large print, audio version and in other languages, please call 0800 073 0510.
Originator: Radiology Department. Date originated: January 2021. Review date: October 2023. Version: 1. DGH ref.: DGH/PIL/02132.
