B4 – Elective surgery
Planned Elective Surgery
Patient Information Leaflet
Introduction
Welcome to The Dudley Group NHS Foundation Trust.
The contents of this booklet will provide you with information and advice regarding your upcoming hospital admission for your planned surgery.
Please read this booklet carefully. It aims to prepare you for your stay and provide you with all the instructions you need for the day of surgery. You may find it helpful to bring this document with you when you are admitted.
If you have any questions about your admission, please contact your consultant’s secretary or specialist nurse who will be happy to help you.
What Happens Next?
Now that you have attended your Pre-operative Assessment appointment, the next step is to await a letter from the consultant’s secretary with your admission details.
Please note that there may be a long wait for your scheduled surgery.
In some circumstances, additional tests or appointments may be required prior to your admission. If required, a member of the Pre-operative Assessment Team will organise this and notify you.
Changes To Your Health
Please inform the Pre-operative Assessment Team if there are any changes to your health or medications prior to your admission date.
Some illnesses increase the risks of anaesthesia and surgery so we may occasionally feel it is safer to postpone your procedure until you are well. The majority of planned procedures can be safely postponed.
Chest Infection
If you have a chest infection which requires antibiotics, we usually recommend waiting 6 weeks between the chest infection resolving and a general anaesthetic. We might continue sooner if we feel the benefits of continuing surgery outweigh the risks of postponing surgery. If you do have a chest infection requiring antibiotics in the 6 weeks before surgery, please contact the Pre-operative Assessment Team who will provide further advice. Contact details are at the end of this booklet.
COVID-19/Colds
If you have had symptoms of COVID-19 or other flu-like illness within 4 weeks of your admission date, please contact the Pre-operative Assessment Team. A runny nose or mild sore throat in the absence of other symptoms is not a concern.
If you have a severe cold or are feverish in the week before surgery, please contact your Pre-operative Assessment Team. Contact details are at the end of this booklet.
COVID vaccinations
If your planned procedure is for a steroid injection under orthopaedics, this will need to be avoided for two weeks before and after the vaccination. If this applies to you, please contact your consultant’s secretary; their contact details will be on your admission appointment letter.
Skin rashes, sores or cuts near the surgical site
If you develop any of these please contact the Pre-operative Assessment Team as this might have implications for surgery. This is especially important in Orthopaedic Surgery where replacement joints are being inserted.
Diarrhoea & Vomiting
Diarrhoea and vomiting can be caused by an extremely infectious tummy bug so if you have had diarrhoea in the 5 days leading up to surgery, please contact the Pre-operative Assessment Team as we may need to arrange another date. We might continue with surgery if the diarrhoea is part of your medical condition.
Cancelling Your Operation
Although every effort is made to keep your date for surgery, there are occasions when we may need to reschedule. We understand that this can be inconvenient for you and will do everything we can to ensure you are given as much notice as possible in this situation. However, due to certain circumstances, we may need to cancel on the day of your procedure.
If you no longer wish to have your operation or you want to reschedule, please telephone your surgeon’s secretary to allow us to offer the slot to someone else. The telephone number will be on the top right hand corner of your admission letter.
Depending on your procedure, you may want extra support or spiritual counselling around the time of your procedure. This can be provided at your request.
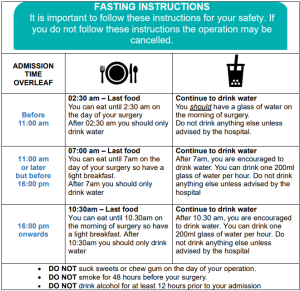
Fasting Instructions
Once your date of surgery is confirmed, please ensure you follow the appropriate fasting instructions detailed. This is very important because if there is food or liquid in your stomach, there is the danger that it could come up into your throat and cause damage to your lungs, being potentially fatal.
If you do not follow the fasting instructions, this could result in your operation being cancelled due to the risk of the above. Your admission letter will provide details regarding your admission time.
If you are unsure as to what time to arrive on your surgery date, please phone your surgeon’s secretary. This number should be on your previous consultant appointment letters.
Medication Advice
A leaflet will be provided by the Pre-operative Assessment Team detailing your individual medication advice, please ensure that the advice is adhered to prior to your admission, failure to do so may cause your surgery to be cancelled.
If you are diabetic, please follow your medication instructions and advice provided in a separate leaflet, given to you at your Pre-operative Assessment appointment.
It is important to continue to take all other medication you are prescribed if they are NOT listed above.
If you have lost the instructions or you have started any new medication since your Pre- operative Assessment appointment, please contact Pre-operative Assessment.
This includes any relevant devices, such as your CPAP machine if you have Obstructive Sleep Apnoea (OSA)
It is particularly important that you are advised by a doctor or nurse about when to restart medications that were stopped before your operation. Please seek advice from your surgical team before you are discharged, if this advice is not given.
Pregnancy & Breast Feeding
Surgery can carry a risk to unborn babies. If you are of childbearing age, a member of staff will ask you to complete a pregnancy test before surgery. The testing will be done in private, and you will be informed of the result. This is a routine test and applies to all women of childbearing age.
Contraception Pill and (HRT)
For most procedures we recommend that you continue taking the pill or HRT. If you are having a major operation or surgery to your legs, then we may need you to stop these medicines for several weeks beforehand. This should have been discussed with you in the surgical clinic and also at your Pre-operative Assessment appointment.
Some medications reduce the effectiveness of the pill for a period of time afterwards. If you are using the pill for contraceptive purposes, please ask the team for advice about the need for using additional protection.
Fitter, Better, Sooner
Getting fit for surgery
It is important your health is optimum before any operation. Stopping smoking, reducing alcohol intake, eating a healthy diet, losing weight and taking regular exercise all help reduce your risk from surgery. To read more about this visit : Preparing for surgery | The Royal College of Anaesthetists.
Wellness Coaching
Our Wellness Coaches offer one-to-one support and advice to help you lead a healthier lifestyle and achieve your goal. From stopping smoking, losing weight, eating more healthily to drinking sensibly or being more active – talking to a Wellness Coach could be just the thing to get you started.
You may also have been invited to join our Surgery Hero Programme, a digital health coaching app to guide you as you prepare for your surgery. Let us know if you would like more information.
NHS Health Check
As you get older, you have a higher risk of developing conditions like high blood pressure, heart disease, type 2 diabetes, and dementia. A free NHS Health Check can spot early signs and help prevent these happening to you, which means you’ll be more likely to enjoy life for longer. If you’re aged 40 to 74, and have not been diagnosed with a medical condition, you may be eligible for a free NHS Health Check. Please contact your GP to arrange this.
Cook 4 Life
Are you looking for quick, easy ideas to help your family eat well on a budget?
Our Cook 4 Life programme will provide you with practical cooking skills and improve your knowledge of healthy eating. You’ll also have fun cooking cheap, tasty and easy dishes, which you can sample and take home.
Nutrition
Eating a balanced diet and working towards a healthy BMI/ weight will always help to minimise complications during and after surgery. You may be asked to drink a carbohydrate rich drink called a ‘pre-op drink’ which contains energy to help you heal afterwards. In the run up to surgery ensure you are eating regular meals with healthy snacks in between. Unless you have been put on a special pre-op diet, please ensure your diet contains:
- 5 items of Fruit and Vegetables per day
- Carbohydrates (i.e., starchy foods), i.e., potatoes, pasta, rice, bread in each meal
- 2 portions of meat, fish, or meat alternatives (i.e., tofu, eggs, or lentils) per day
- 2-3 portions of milk and dairy products (i.e., yoghurt, milk, or cheese) per day
- Drink 6-8 cups of fluid per day
Shape up 4 Life
Do you want to lose weight and keep it off long-term? Our Shape Up 4 Life classes will help you manage your weight through balanced nutrition and simple exercises. Through group support, you’ll receive advice and encouragement to make healthy lifestyle choices, together with light physical activity with a qualified instructor.
Smoking
We recommend you stop smoking as early as possible prior to surgery to help reduce the risk of postoperative complications. Stopping smoking 4 weeks before surgery will help with wound healing and your heart and lung function. Even stopping 3 days before will help your body transport more oxygen. Speak to your GP or local pharmacy for more help. You are far more likely to quit successfully with help and support from a trained advisor. Offering expert advice, support, and encouragement our advisors will help you stop smoking for good. They’ll also be able to tell you about nicotine replacement products and other stop smoking medicines that can help.
The NHS Stopping Smoking helpline is 01384 732402 or email letsget.healthydudley@nhs.net. These recommendations also apply to second hand smoke, as exposure to this can still put you at risk. Try to avoid being around anyone smoking in the run up to your surgery. The hospital and its grounds are strictly non-smoking. This includes the canopies at the entrances to the building. There is a 15 m exclusion zone around the premises where smoking is not permitted. Designated smoking shelters are available.
Alcohol
There is a link between hazardous drinking and complications such as bleeding, impaired wound healing, and infection after surgery. Avoiding alcohol in the weeks before surgery will significantly reduce the risk of these serious complications from occurring. For most people stopping drinking will cause no problems at all. However, if you are a heavy drinker and have had anxiety, tremor, or confusion when you stop drinking then suddenly stopping is not advised. The body can become dependent on alcohol and suddenly stopping can cause seizures and/or death. If you are a heavy drinker who has had problems when you’ve stopped in the past, please seek further advice from your doctor or nurse. Men and women are advised not to drink more than 14 units a week (equivalent to 6 pints of average strength beer or 10 small glasses of low strength wine)
Recreational Drugs
Recreational ‘street drugs’, including legal highs, can cause serious and possibly life-threatening reactions under anaesthetic. Please advise us of any drug usage so that we can make a plan to ensure your procedure is carried out as safely as possible. For free confidential advice about using drugs please see www.talktofrank.com

Preventing Blood Clots in Hospital (VTE)
This section is about a condition called Venous Thromboembolism (VTE). It gives information on what VTE is, what causes it, how it is treated and what can be done to help reduce the risk of getting it.
What is a venous thromboembolism (VTE)?
It is a term for both ‘deep vein thrombosis’ (DVT) and ‘pulmonary embolism’ (PE).
Deep vein thrombosis (DVT)
A DVT is a blood clot in the deep veins. This is most commonly in the lower limbs but can occur in any deep vein.
Pulmonary Embolism (PE)
A PE is when all or part of the DVT breaks off, travels through the body and blocks the blood vessels to the lungs. This is potentially life threatening. You can have a PE without experiencing signs and symptoms of a DVT.
What causes a VTE?
One of the most recognised risk factors is admission to hospital. Because of this, you will have an assessment of your individual VTE risk on admission. This will be reviewed throughout your hospital stay as required.
What are the signs and symptoms of VTE?
One of the most recognised risk factors is admission to hospital. Because of this, you will have an assessment of your individual VTE risk on admission. This will be reviewed throughout your hospital stay as required.
- Swelling, usually in one leg.
- Tenderness of the leg muscles, often the calf muscles.
- Reddish or bluish skin discoloration.
- A leg that is warm to touch.
- Sudden shortness of breath.
- Chest pain that is sharp or stabbing and that may get worse on breathing in.
- Rapid heart rate.
- Unexplained cough, sometimes with bloody mucus
Risk assessment for VTE
Who will be risk assessed?
All adult patients admitted to hospital including patients having certain day case procedures (procedures where you will only be in hospital for the day) will have a VTE risk assessment.
When will I be risk assessed?
A member of the clinical team will carry out your risk assessment when you are admitted to hospital. This will be reviewed within 24 hours of admission and whenever your clinical condition changes. If you are having a planned operation, the risk assessment is sometimes carried out during your Pre-operative Assessment appointment. In this case, you will be checked for any changes on the day of admission.
How will I be risk assessed?
The clinician will complete an assessment based on your medical condition. Other factors such as age, weight and previous personal or family history of VTE are included in this assessment. If you are considered to be at risk of VTE, you will be given treatment to try and prevent it.
If I need preventative treatment, what will it be?
Anticoagulants (blood thinners): most patients at risk will be prescribed a small dose of an anticoagulant. The most commonly used one is heparin which is a small injection given in the skin over the tummy. Not all patients will be given heparin.
Anti-embolism stockings: if suitable, you will be measured and fitted with these. It is very important to wear them as instructed and ensure that they are taken off at least once a day so that your skin can be washed and inspected. Most people who require stockings will have had surgery. Intermittent pneumatic compression: Intermittent pneumatic compression (IPC) devices are used to help prevent blood clots in the deep veins of the legs. These devices use cuffs around the legs that inflate and deflate, squeezing your legs. This increases blood flow through the veins of your legs and helps prevent blood clots. Most people who require IPC will have had surgery or a stroke. Before any of these treatments are prescribed, the clinician will check if there are any reasons why you should not have them.
What can I do to help reduce my risk of VTE?
There is a lot that you can do yourself to reduce your risk of developing VTE:
- When you are able to drink, ensure you drink plenty to keep hydrated.
- Keep moving and walk as soon as you are advised to.
- Ask your doctor or nurse “What is being done to reduce my risk of blood clots?”
Travelling Abroad
If you have a flight longer than 4 hours either 4 weeks before or 4 weeks after your surgery, please inform your surgeon’s secretary. Some operations may need to be re-scheduled to reduce the risk of developing a blood clot.
For major operations on the leg or pelvis (i.e., joint replacement) it might be necessary to defer flights for up to 12 weeks after surgery. Each case is unique and if the benefit of continuing surgery is thought to outweigh the risks it might be appropriate to proceed. If you are flying after surgery, please seek advice about reducing the risks of blood clot from your doctor and inform your travel insurance company.
What happens when I leave hospital?
For some people, it may be necessary for treatment to carry on after you leave hospital. If this is the case, this will be explained to you. If you develop any signs and symptoms of VTE at home, please seek medical advice immediately, either from the ward that discharged you, your GP or your nearest hospital emergency department.
Pain relief
Non-prescription painkillers, e.g., paracetamol and ibuprofen (if safe for you) can be purchased cheaply in many places such as supermarkets. We do not usually supply simple over the counter medicines (i.e. painkillers) so please ensure you have obtained a supply before your procedure. The nurses in Pre-operative Assessment Team can advise you regarding which painkillers are suitable and safe if you’re unsure.
What types of pain relief are there?
Pain medication can be given in various forms depending on your condition and the type of surgery you have had. They include:
Medication by mouth This will either be in the form of tablets, liquid, or dissolvable preparations, given regularly or when you need them.
Intramuscular injection This will be given by injection into a large muscle such as the thigh. It is used if patients are being sick or feeling extremely sick.
Intravenous injection This will be given through a small plastic tube (cannula) straight into a vein for rapid pain relief. If you have had surgery, you may already have a cannula in place. The cannula can also be used to give anti-sickness medications for patients who are feeling sick or being sick.
Patient-controlled analgesia (PCA) This is a pain relief pump controlled by the patient. It is programmed to allow you to deliver pain medication when you need it and has safety features to prevent harm (we have a separate information sheet about this).
Epidural This is a pain relief pump used to deliver continuous pain medication through a catheter (small, plastic tube) in the spine (we have a separate information
Local wound infiltration This is a pain relief pump that delivers continuous pain medication to the site of the operation. It is only used in a selection of operations.
What happens after my operation?
When you wake from your anaesthetic in the recovery area, we will ask you about your pain and what it is like. This is best time to treat pain and you will get maximum benefits from the pain relief if it is given at this stage.
When you arrive on the ward, nurses will ask about your pain regularly and give you the pain relief that you have been prescribed. Good pain relief means that you will recover quicker from surgery. This will enable you to get up and about and carry out your daily activities sooner.
Can I ask for help?
If your pain control is not adequate at any time and you are still feeling pain, or if you have any questions or concerns about your pain relief, please ask the nurse. It is best to do this as soon as you can to enable us to respond quickly. If appropriate, a member of the pain team will visit you to discuss this.
Children
Prior to admission, you may visit the Children’s Ward to allow your and your child to familiarise themselves with the ward and nursing staff. This can be arranged on weekdays between 09:00 and 15:00 and will be led by our Play Specialists. Please telephone the ward on 01384 244271 if you wish to arrange this.
You may be a while waiting for your theatre slot so bring a favourite toy, book, game or comforter. Children are prioritised at the start of the list where possible.
General Information for the day of Surgery
- Please bring all prescribed medication with you for your admission, except controlled drugs.
- You should take all your regular medication as normal unless instructed otherwise.
- Except in exceptional circumstances, relatives are not allowed through to the day case ward area.
- You will not be able to drive yourself home or use public transport after your procedure, so you will need to arrange for someone to collect your from hospital.
- Unless you have made special arrangements with the Pre-operative Assessment Team, after day case surgery, you will require a responsible adult to stay with your for the first 24 hours. Please let us know if this is an issues for you.
- Theatre lists can run all-day. The final order of the theatre list is decided on the morning of the surgery by the surgeon, anaesthetist and the theatre team. If you are later on the list, we will allow you to have further drinks of water on the ward.
- If you are staying overnight, we will identify the ward you are going to on the day of surgery.
- On the ward the nurse will talk through the admission process and get you ready for surgery.
- You will meet and talk about your surgery with the surgeon and anaesthetist.
- We cannot take responsibility for monies or valuables in your possession or the possession of anyone accompanying you, while you are in hospital and we would, therefore, advise you to leave valuables, jewellery, and body piercings at home.
- You do not have to remove your wedding ring, but it will need to be covered with tape once you arrive.
- Please remove all make-up and nail varnish. Acrylic nails may be left on but please check with nursing staff when you arrive.
- It is hospital policy to offer all female patients between the ages of 15 and 55 a pregnancy test on the day of surgery.
- If you require any further information about your admission or you are unsure of any of the above, please contact Pre-operative Assessment Team in the first instance. In some instances, we may refer your query to the surgeon’s secretary.
Support for additional needs
We aim to deliver high quality; person-centred, safe acute hospital services for people with additional support needs. Specifically, we can assist patients with memory or cognitive impairment, including dementia or a learning disability. The Trust have a dedicated teams and their contact details are:
- Learning Disabilities Team to support patients with learning disabilities along with their families/carers. They can be contacted on 01384 456111 extension 4205 (Monday to Friday 8am to 4pm).
- You can contact the Pre-operative Assessment Team on 01384 456111 extension 3301.
Your Anaesthetic
We are proud that The Dudley Group Anaesthetic Department is accredited by the Royal College of Anaesthetists. You will meet your anaesthetist on the day of surgery who will discuss an anaesthetic plan with you. Options may include a general anaesthetic (going to sleep), sedation (which gives a sleep-like state) or regional anaesthesia (when an injection is used to numb part of the body). These may have been discussed at your Pre-operative Assessment appointment.
For patients | The Royal College of Anaesthetists
If you have any questions, or if there is anything you do not understand about this leaflet, please contact:
Pre-operative Assessment
Russells Hall Hospital switchboard number: 01384 456111 ext 3301
If you have any feedback on this patient information leaflet, please email dgft.patient.information@nhs.net.
Date reviewed: October 2025 Next review date: October 2028 Version: 1
