General Surgery
Tracheostomy
Patient Information Leaflet
Introduction
This leaflet is for patients having a tracheostomy and their relatives. It gives information on the procedure, and its benefits and risks.
What is a tracheostomy?
A tracheostomy is a tube that goes into the windpipe (trachea) through the neck – please see Figure 1. It is usually put in by intensive care doctors in the Critical Care Unit or by surgeons in operating theatres.
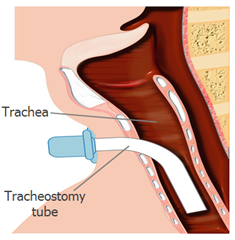
Figure 1 shows a tracheostomy tube going in through the neck.
What are the benefits of a tracheostomy?
The benefits are:
- To reduce the risk of food or fluid going into the lungs if people find coughing difficult.
- To deliver oxygen to the lungs when a person is unable to breathe normally after an injury or accident, or because their muscles are very weak.
- To allow a person to breathe if their airway is blocked. This can be caused by such things as swelling or a tumour.
- A tracheostomy tube is more comfortable for most people than having a tube in their mouth. It means that sedating medicines can usually be reduced or stopped.
- It is easier to breathe through a tracheostomy tube than a mouth tube.
In many cases, a tracheostomy will be planned in advance although sometimes it may need to be carried out in an emergency.
How is a tracheostomy put in?
Patients will be given either a general anaesthetic (where they will be asleep) or a local anaesthetic. This will depend on their condition but if done in Critical Care the patient will be asleep. The operator will then make a cut in the front of the neck and create an opening. A hollow, removable tube is inserted through the opening and secured in place. The tube consists of an outer and an inner tube.
What are the risks of a tracheostomy?
Although the procedure is normally safe, as with many medical procedures, it does carry some risks. The risks will depend on:
- The age and general health of the patient.
- The reason the tracheostomy is needed.
Early problems can include:
- Bleeding – This will be investigated and the cause of it will be treated.
- Low oxygen levels – Again, this will be investigated and the cause of it will be treated.
- Punctured lung (pneumothorax) – If this happens, air escapes from the lung. This air then fills the space outside of the lung, between the lung and chest wall. The build-up of air puts pressure on the lung so it cannot expand as much as it normally does when a breath is taken.
Treatment for this will depend on the patient’s condition and how large the lung injury is. A small puncture in the lung is often treated by oxygen therapy and will be monitored, as it sometimes corrects itself. For larger punctures, a chest drain can be used to drain out excess air. If the puncture is very large, this may need surgery. In this case, the patient will be referred to a specialist.
Later problems can include:
- The inner tube can come out – if this happens, the inner tube can be replaced.
- The inner tube can become blocked – again, if this happens, the inner tube can be replaced.
- Narrowing of the windpipe – in this case, the patient would be referred to a surgeon. Surgery may be needed to widen the windpipe.
Although rare (1 in 500), there is a risk of death associated with a tracheostomy. However, it can be difficult to know whether the cause of death is from the tracheostomy or from the patient’s medical condition, which is often critical.
What are the alternatives to a tracheostomy?
An alternative is to have a tube in through the mouth. However, this can lead to damage to the vocal cords, mouth and lips. It also means sedative drugs will be needed as mouth tubes are usually uncomfortable.
What happens afterwards?
Most tracheostomies put in in Critical Care are only in for a short amount of time. When they are no longer needed, we remove the tube and put an air-tight dressing over the cut. Usually the wound will close naturally and heal, leaving a small scar on the neck. If the wound does not close naturally, we may possibly need to put stitches in it.
Is consent needed for tracheostomy?
If possible, the doctors will get consent from the patient. However, this is not usually possible for patients in Critical Care as they are either too unwell or receiving sedating medicines. In this case, at least two senior doctors will make a decision, acting in the best interests of the patient.
Before the procedure, the doctors will explain the reasons for the tracheostomy and how it is carried out with the patient’s next-of-kin, family or advocate This gives them a chance to ask questions. However, adults cannot give consent on someone else’s behalf unless they have been given special legal rights, called a power of attorney.
Can I find out more?
You can find out more from the following weblink:
NHS Choices
http://www.nhs.uk/Conditions/Tracheostomy/Pages/Complications.aspx
If you have any questions, or if there is anything you do not understand, please contact the Russells Hall Hospital switchboard number on 01384 456111 and ask for the relevant department who issued this leaflet. If you have any feedback on this patient information leaflet please email dgft.patient.information@nhs.net
This leaflet can be made available in large print, audio version and in other languages, please call 0800 073 0510.
Originator: Gagandeep Panesar, CT Anaesthetics. Reviewed by: Dr David Stanley, Consultant, Critical Care. Date reviewed: August 2025. Next review due: April 2027 Version: 4. DGH ref: DGH/PIL/01101.
